Sunday, July 25, 2010
D-Day has come !!
Both me and Mamma are a bundle of nerves now !
Dad is busy doing the required running around the hospital and following up with my doctor aunty.
Gosh! I am both excited and scared at the same time .
I havent had much exposure to the 'external' world you know :) I was sort of getting into a comfort zone inside Mamma.
Wish me , Mamma and Daddy luck .
My next post will take sometime as I get accustomed to the external world .
I promise to share with you quite a few pics ( Dad is charging the camera as we speak :))
Goblu
Tuesday, July 6, 2010
Signs of Premature Labor:
If you start having regular contractions that cause your cervix to begin to open (dilate) or thin out (efface) before you reach 37 weeks of pregnancy, you're in preterm labor, also known as premature labor. If you deliver your baby before 37 weeks, it's called a preterm birth and your baby is considered premature.
About a quarter of all preterm births are intentional. For example, your medical team might decide to induce labor early or perform a cesarean section if you have a serious medical condition such as severe or worsening preeclampsia or if your baby has stopped growing.
The rest are known as spontaneous preterm births. You may end up having a spontaneous preterm birth if you go into labor prematurely, if your water breaks early (called preterm premature rupture of the membranes or PPROM), or if your cervix dilates prematurely with no contractions (called cervical insufficiency).
About 12 percent of babies in the United States are born prematurely. This number has gone up over the years, partly because more women are pregnant with twins or higher order multiples, who tend to arrive early.
Preterm birth can cause health problems or even be fatal for the baby if it happens too early. The more mature a child is at birth, the more likely it is that he will survive and be healthy.
Premature babies born between 34 and 37 weeks generally do very well. If you go into labor before 34 weeks, your medical team may be able to delay your labor for a few days so your baby can be given corticosteroids to help his lungs develop faster, which increases his chance of survival.
http://www.babycenter.com/
Preterm Labor Signs and Symptoms
Premature labor, also known as preterm labor, is a very serious complication of pregnancy. This is defined as labor that begins prior to 37 weeks gestation. Unfortunately, many women do not understand the signs of premature labor. Early detection can help prevent premature birth and possibly enable you to carry your pregnancy to term or to give your baby a better chance of survival.
Signs of Premature Labor
Call your practitioner if you have any of the following:
* Contractions or cramps, more than 5 in one hour
* Bright red blood from your vagina
* Pain during urination, possible urinary tract, bladder or kidney infection
* Sudden gush of clear, watery fluid from your vagina
* Low, dull backache
* Intense pelvic pressure
Prevention of Preterm Labor
While not all cases of preterm labor can be prevented there are a lot of women who will have contractions that can be prevented by simple measures.
One of the first things that your practitioner will tell you to do if you are having contractions is staying very well hydrated. We definitely see the preterm labor rates go up in the summer months. What happens with dehydration is that the blood volume decreases, therefore increasing the concentration of oxytocin (hormone that causes uterine contractions) to rise. Hydrating yourself will increase the blood volume.
Others things that you can do would be to pay attention to signs and symptoms of infections (bladder, yeast, etc.) because they can also cause infections. Keeping all of your appointments with your practitioner and calling whenever you have questions or symptoms. A lot of women are afraid of "crying wolf," but it is much better to be incorrect than to be in preterm labor and not being treated.
Management of Preterm Labor
There are a lot of variables to managing preterm labor, both in medical options and in terms of what is going on with you and/or your baby.
Here are some of the things that you may deal with when in preterm labor.
* Hydration (Oral or IV)
* Bedrest (Home or Hospital), usually left side lying
* Medications to stop labor (Magnesium sulfate, brethine, terbutaline, etc.)
* Medication to help prevent infection (More likely if your membranes have ruptured or if the contractions are caused by infection)
* Evaluation of your baby (Biophysical profile, non-stress or stress tests, amniotic fluid volume index (AFI), ultrasound, etc.)
* Medications to help your baby's lung develop more quickly (Usually if preterm birth in inevitable)
Preparation for preterm birth
The best key is always prevention and early detection. Make sure to ask your practitioner to discuss the signs and symptoms of preterm labor to you and your partner at your next visit.
http://pregnancy.about.com/od/pretermlabor/a/pretermlabor.-KJn.htm
Risk factors associated with premature labor
Some risk factors have been associated with a higher chance of premature labor. However, just because you have some risk factors does not mean that you will experience premature labor. Review the following risks factors and let your health care provider know if any apply to you.
Possible risk factor for premature labor:
- Premature labor or delivery during a previous pregnancy
- Misshapen uterus
- DES (Diethylstilbestrol) daughter (If your mother was prescribed this medication during her pregnancy to prevent miscarriage, you are considered a DES daughter. DES has been linked to shortening of the cervix.)
- Abdominal surgery during pregnancy and/or cervical cerclage (a stitch in your cervix)
- More than two second trimester miscarriages or elective abortions
- Previous Cone Biopsy or LEEP (procedures used to diagnose and/or treat the cervix of women with abnormal Pap tests)
- Carrying more than one baby
- Dehydration
- History of cervical change and/or excessive uterine contractions at less than 33 weeks in a previous pregnancy
- Serious infections with fever (greater than 101 degrees Fahrenheit) during this pregnancy
- Recurring bladder and/or kidney infections
- Excessive amount of amniotic fluid
- Unexplained vaginal bleeding after 20 weeks of pregnancy
- Using recreational drugs, such as cocaine or amphetamines
- Domestic violence
- Smoking more than 10 cigarettes per day
- Extreme emotional or physical stress
Fetal Development:34 weeks
Your amazing baby is on the move! They’ve been riding fairly high in your stretched-out womb till now (while kindly compressing your poor internal organs), but now they’re planning on making the big move to your pelvis this week. If you haven’t noticed it already, you’ll be feeling the weight shift that signals that your baby is most likely out of breech position, with their head now resting on your pubic bone. In liver news: although not quite fully formed, your little miracle’s liver is now capable of processing a certain amount of waste. In general, most of your child’s prenatal physical development is pretty much up to snuff and ready for the outside world. Naturally, further weight gain is expected—so you’re still not at maximum capacity despite probably feeling like you definitely are maxed out.
And how's mom doing?
Obviously the big change for you is the notable weight shift (known as “lightening” or “engagement”). Now that your baby is resting deeper in your pelvis, you may find yourself walking as if you're carrying a watermelon between your legs. Yes dear, you’re officially “waddling” these days. Try to comfort Now that your baby is resting deeper in your pelvis, you may find yourself walking as if you're carrying a watermelon between your legs yourself with this thought: it’s nearly over. Soon, you’ll just have to carry your adorable little watermelon in your arms. And in a rare spate of good news: this weight shift means you can breathe easier now that your lungs aren’t compressed. The not-so-good news, it’s a trade off: (we’ll wait till you’re back from the restroom) this new position has your poor bladder even more squished than before. We’d recommend writing your bladder little love poems to convince it not to leave you altogether, but unfortunately bladders don’t speak English (only Italian love poems will do).
If you've recently noticed some less-than-appealing itchy red bumps on your belly (and possibly around your thighs and belly), you've got yourself a harmless but not fun round of pruritic urticarial papules and plaques of pregnancy (PUPPP if your don't have the patience for the full name). If you feel itchy ALL over your body, that's different, and you should call your health care practitioner as this could be a liver problem.
At your next check up you can expect your physician to conduct a Group B Streptococci test (GBS), a common bacteria screening. As long as you have a strong immune system, you’re in the clear (one more reason to eat right and exercise!), but your little one is more susceptible to serious health complications (including meningitis, pneumonia and blood infection) if not diagnosed and treated properly—so the tests are good for some peace of mind. Hang in there momma, you’re already a super-star for making it this far!
http://pregnancy.baby-gaga.com/calendar
Baby
Besides looking like a newborn at 34 weeks of pregnancy, your baby is acting like a newborn as well. Her eyes open when she’s awake and close when she is sleeping. Her sleeping cycles are the same now as they will be when she is born. She has learned to blink and can see better when a bright light is shined on your stomach. She recognizes voice and sound patterns from the outside world and is most comforted by the sound of your voice.
She weighs about 4 ¾ pounds now and is about 18 inches long. Her fingernails have reached the end of her fingertips at week 34 of pregnancy and she may even scratch her face before she is born. Her fat layers are growing every week to fill up that wrinkly skin and she may have already turned into the head down position for labor.
Your baby’s central nervous system is still maturing, and her lungs are almost fully ready to breathe air. If your baby is born this week, she has a 99% chance of survival outside of the womb, pretty darn good odds.
Mom
The last few weeks can be uncomfortable and tiring. The weight of your baby and your body may start to leave you feeling fatigued at week 34 of pregnancy. Be sure to rest up and save some energy for the big day. In the next couple of weeks, you will most likely be tested for Group B streptococcus (GBS). GBS is a type of bacteria that some pregnant women carry in their vaginal or rectal areas. This bacteria is harmless to you, but can be transmitted to your baby during childbirth and cause some complications like meningitis, bacterial blood infections, and pneumonia. If you test positive for GBS, your doctor can prevent many of these complications by administering an antibiotic to you through IV during labor.
As you get closer to your labor day, have you thought about how this baby will affect your relationship? If this is your first baby, a new member to the family can be exciting, but overwhelming. If you are married or living with your partner, having that first baby can strengthen your relationship greatly. On the other hand, if you have already had some differences, a baby can add even more stress. The key to a great relationship with your partner is good communication.
What often happens with first babies is that one parent is more ready and willing to quickly transition their lifestyle than the other. Add to that the stress of decreased sex, little sleep, and a high maintenance baby that takes all of your energy and focus. It’s no wonder that relationships can be a bit strained that first year.
Be proactive and make a commitment to your partner. Commit to weekly or at least monthly dates with just the two of you, no baby. If you are low on cash, a picnic or a hike will do fine. OR take baby to a babysitter and cook yourselves a romantic dinner.
When conflicts arise, talk them out before resentments show. Try and get your partner involved with the baby as much as possible. If you are nursing, let dad bathe the baby. Anyway you can get him to bond to baby will help him bond with the family lifestyle. Remember that bonding is harder for dad at first; he didn’t carry your child for nine months, he’s not able to nurse, and babies naturally bond to mom first.
Encourage your partner’s dad skills by encouraging him to participate more. While your baby’s first year can be a challenge, with hard work and dedication, you will discover more love than you have ever known, from your partner and your child.
http://smartmomma.com/pregnancy/
Week 34 Pregnancy Symptoms
Flatulence: As your third trimester progresses, you may be getting gassier. Anxiety just makes those gassy feelings worse — you tend to swallow more air when you’re stressed — so try this tension tamer: Breathe deeply through your nose and out through your mouth for a minute or two each day.
Constipation: Need to rev up those slow-moving bowels? Rough up your diet with some dried fruits, fruits and veggies, and whole grains. One thing you don’t want to do — take laxatives (even herbal ones). Get your practitioner on board before taking any medicine for constipation.
Increased vaginal discharge: As your pregnancy progresses, you could see an increase in vaginal discharge. Blame pregnancy hormones (especially estrogen) for this symptom — they increase blood flow to the pelvic area and stimulate the mucous membranes (making your juices flow). Wearing undies with a cotton crotch can keep you drier (and that can curb odors).
Hemorrhoids: Constipation’s almost constant sidekick? Hemorrhoids. These pesky piles can be kept to a minimum by doing Kegels, which can improve circulation to the area.
Backaches: Your shifting center of gravity from back to belly puts more pressure and (ouch!) pain on your lower back. There are many solutions to cure your aching back, so if one doesn’t work, another most certainly will. One to try: Take a break and stretch, stand, or walk. Sitting too long can make your back hurt even more.
Leg cramps: Leg cramps are most common around now, when the three main culprits — pregnancy weight, swelling, and fatigue — are at their peak. If you feel a spasm, try standing on a cold surface (that can sometimes stop one).
Stretch marks: If you’re fair-haired and have a genetic predisposition toward stretch marks, you’re more likely to get them than someone who’s darker-haired (or skinned). But no matter what your skin or hair color, you can try to keep these classic marks of maternity to a minimum by keeping your weight gain slow and steady.
Mild swelling of ankles and feet: As you get bigger and your body tissues accumulate and retain fluids, you may experience swelling in your ankles, feet, and fingers. Slipping into comfy slippers at the end of the workday can help soothe your swollen tootsies.
Hair changes: You knew your hair would grow faster and more lustrous while you were pregnant, but you probably didn’t expect it to grow in places you weren’t expecting — like your cheeks, chin, and back. Waxing is safe during pregnancy; but since skin is extra-sensitive now, ask for a formula for sensitive skin.
Shortness of breath: As your pregnant belly gets bigger, your lungs won’t be able to expand as fully, so you may feel winded, even after a trip to the bathroom. Sleeping propped on your left side can help at night, and just take it easy.
Difficulty sleeping: If you’re not worrying about your impending D-day, then leg cramps and trips to bathroom are banishing any chance of shut-eye. Try lulling yourself to sleep with a warm bath and a cup of warm milk and read a book or listen to music instead of surfing the net or watching TV (those activities can keep you up).
Leaking colostrum: As your due date approaches and the third trimester wears on, your breasts may leak colostrum — yellowish pre-milk that will be your baby’s first drink. You won’t be leaking more than a few drops, but if you feel uncomfortable, try nursing pads.
http://www.whattoexpect.com/pregnancy/week-by-week/Fetal Development:33 weeks
- The baby is now 4.4 pounds (2 kg) and around 17.5 inches (44cm) in length.
- The diameter of the head is about 8.5cm.
- The baby fuzz, lanugo, is disappearing.
- Your baby drinks about a pint of amniotic fluid a day.
- You may gain a pound a week (500g) for the rest of your pregnancy.
- Half of your weight gain will go directly to your baby.
You may gain a pound a week for the rest of your pregnancy. Do not stop eating or start skipping meals as your weight increases. Both you and your baby need the calories and nutrition you receive from a healthy diet. Calcium intake is extremely important during pregnancy because the baby will draw calcium from the mother to make and harden bone. This can greatly weaken her own bones and teeth because the developing fetus will take minerals from the mother's skeletal structure as needed.
http://www.baby2see.com/development
Fetal development in pregnancy week 33:
For all the weight and bulk you’re lugging around these days, you’d think your little champ should weigh much more than a mere 5 lbs and measly 17 inches in height, but nope, that’s about the average size for a baby in its thirty-third week. In terms of appearances, they’re getting cuter and pudgier every minute as they pile on the baby fat for those adorable little wrist rolls and chubby toes. And as we’re sure you’ve already noticed they’re getting stronger with every passing day. Nowadays, it’s possible to observe a well-placed kick just by watching your belly—but you already knew that didn’t you? Although they’re getting stronger, your bigger-by-the-day baby is losing space to move around, so the actual rate of movement will drop off in the last few weeks, despite that powerful drop-kick they’ve been working on. Hey, did you know you’ll continue feeling their movements even during labor?
And how's mom doing?
Here’s a good way to deal with your mounting impatience: map out your plan of action for the big day. It’s an important and necessary step that’s also pretty soothing and fun. So, get out a piece of paper and pen. If you think about it, planning all the details now can be a real saving grace once Massaging the perineum (the area around the vagina) can reduce your chance of it tearing during delivery the chaos and pain of labor starts up. This would include having a packed bag with a change of comfortable clothes, reading material, maybe an i-pod and your camera or camcorder (whichever you decide, if any at all). Know your driving route to the health center. Or if you’re delivering at home, make sure you have the delivery room prepared (equipped with your most favorite soothing music), and all necessary instruments and materials ready for use. Of course, get your doctor or midwife on speed-dial. Massaging the perineum (the area around the vagina) can reduce your chance of it tearing during delivery and there’s no time like the present to start. Be on your toes (not literally, just mentally) as it's now totally conceivable you might have to spring into action any day! Then again, it might still be another seven weeks.
http://pregnancy.baby-gaga.com/calendar/week33
Friday, July 2, 2010
Recovering from a cesarean delivery:
Like any new mother, you'll probably feel both euphoric about and overwhelmed by the new person in your arms. But you'll also be recovering from major abdominal surgery while dealing with typical postpartum issues such as engorged breasts, mood swings, and vaginal discharge.
C-section patients typically stay just three or four days in the hospital before going home. But your recovery will be measured in weeks, not days, so once home you'll need help taking care of yourself and your new baby. What's more, if you have other children, they may be feeling needy after you've been away from them for a few days, to say nothing of the fact that you're returning home with a new baby! Plan to get all the help you can.
What will I get for postpartum pain relief?
If you have an epidural or spinal for your c-section, your anesthesiologist may add morphine, which can provide excellent postpartum pain relief for up to 24 hours without the grogginess that you get from systemic narcotics. Some anesthesiologists leave the epidural in for 12 to 24 hours after surgery so you can get more medication through it if needed.
Once your regional analgesia is no longer providing adequate pain relief, you'll be given systemic pain medication, usually pills containing a narcotic and possibly acetaminophen. It may help to take ibuprofen, too. You'll also be given a stool softener to counteract the constipating effect of the narcotic.
If you have general anesthesia for your surgery or you don't get a dose of morphine through your spinal or epidural afterward, you'll be given systemic narcotics for immediate postpartum pain relief. You'll either get a shot of pain medication every three to four hours or you'll use a system called "patient-controlled analgesia": You push a button when you're feeling discomfort that delivers medication through your IV. A machine controls the doses so you don't get more than what's safe.
In any case, don't be shy about asking your nurse for more medication if you're uncomfortable. You don't need to suffer in silence, and the longer you wait to ask for the medication you need, the harder it is to control pain in the end.
If the medication that's been ordered for you isn't covering your pain, let your nurse know. If the nurse can't help you, ask to see an obstetrician or anesthesiologist. The more comfortable you are, the easier it'll be to breastfeed your baby and to get moving again.
What's recovery like during the first few days?
You may feel groggy and possibly nauseated right after surgery. Nausea can last up to 48 hours, but your caregiver can give you medication to minimize your discomfort. Many moms also feel itchy all over, particularly those who received narcotics in their epidural or spinal. If this happens to you, let your caregiver know so she can give you medication to relieve the itchiness.
If you plan to breastfeed, you can start in the recovery room right after surgery. Ask the nurse to show you how to nurse in the side-lying position or using the football hold, so there won't be pressure on your incision.
Breastfeeding can be challenging in the days after a c-section because of the pain from a healing incision. Ask to see a lactation consultant as soon as possible to help you position your baby comfortably so you don't end up with sore nipples. If the hospital doesn't have a lactation consultant, ask for the nurse who's the resident expert.
You may feel numbness and soreness at the incision site, and the scar will be slightly raised, puffy, and darker than your natural skin tone.
Your doctor will come by daily to see how you're doing and check that the wound is healing properly.
Anything that puts pressure on the abdominal area will probably be painful at first, but you'll feel a bit better day-by-day. Be sure to use your hands or a pillow to support your incision when you cough, sneeze, or laugh.
Your nurse will come by every few hours at first to check on you and help you. She'll take your vital signs, feel your belly to make sure your uterus is firm, and assess the amount of vaginal bleeding. Like any woman who just delivered a baby, you'll have a vaginal discharge called lochia, which consists of blood and sloughed-off tissue from the lining of your uterus. For the first three or four days, it will be bright red.
Your nurse will also instruct you on how to cough or do breathing exercises to expand your lungs and clear them of any accumulated fluid, which is particularly important if you've had general anesthesia. This will reduce the risk of pneumonia.
If everything's okay, your nurse will remove your IV and urinary catheter, usually within 12 hours of surgery, and you'll likely be able to start eating bland, mild foods if you feel like it.
You might have some gas pain and bloating during the first two days. Gas tends to build up because the intestines are sluggish after surgery.
Getting up and moving around will help your digestive system get going again.
If you're in great discomfort, the nurse may give you some over-the-counter medication that contains simethicone, a substance that allows gas bubbles to come together more easily, making the gas easier to expel. Simethicone is safe to take while breastfeeding.
You may be encouraged to get out of bed the day of surgery and certainly by the next day. (Do not, however, attempt to get up by yourself.
The nurse should be at your side the first time.) In the meantime, get the blood going in your legs by wiggling your feet, rotating your ankles, and moving and stretching your legs.
Just walking to the bathroom may seem impossible at first, but moving around is important for your recovery. It will help your circulation and make it much less likely that you'll develop blood clots. What's more, it will make your bowels less sluggish, which will help you feel a whole lot more comfortable sooner.
It's also important to get to the bathroom to urinate regularly. A full bladder makes it harder for the uterus to stay contracted and increases pressure on the wound.
By the second day, you should be taking a couple of short walks with help from your partner or a nurse. Try to take your walks a short time after you've taken pain medication, when you're likely to feel more comfortable.
In three to four days, your doctor will probably remove your sutures or staples. This takes just minutes, and you may feel a small pinch but no pain. After that, if all's well, you'll be sent home.
What's recovery like after I leave the hospital?
Expect to need help – and lots of it – once you get home. If nobody offers, ask for support from your partner, parents, in-laws, and friends.
If you're worried that you may not have enough support, hire paid help if you can afford it.
You'll likely be given a prescription for more painkillers and a stool softener before you leave the hospital. You may need prescription painkillers for up to a week after surgery, gradually transitioning to over-the-counter pain relievers. (If you're breastfeeding, don't take aspirin or drugs containing acetylsalicylic acid.)
Drink plenty of fluids to help you avoid constipation. Your incision will likely feel better day-by-day, quite noticeably so after several days, though it may continue to be tender for several weeks.
Call your caregiver if you have signs of an infection, including:
* warmth, redness, or swelling at the incision site
* oozing from the incision site; worsening or sudden onset of pain
* any fever (even if your incision looks fine)
Your vaginal bleeding and discharge should be diminishing, though it may last up to six weeks. It should gradually turn from bright red to pink and then yellow-white. If menstrual-type bleeding continues past the first four days after delivery or comes back after slowing, call your healthcare provider.
For more information on warning signs of a medical problem in the weeks after delivery, see our article on when to call your practitioner.
How active should I expect to be?
While it's essential to get plenty of rest once you're home, you also need to get up and walk around regularly. Walking promotes healing and helps prevent complications such as blood clots. But don't overdo it.
Start slowly and increase your activity gradually. Since you're recovering from major abdominal surgery, your belly will feel sore for some time. Take it easy and avoid heavy household work or lifting anything heavier than your baby for eight weeks.
In six to eight weeks, you'll be able to start exercising moderately – but wait until your caregiver gives you the go-ahead. It may be several months before you're back to your former fit self. You'll be able to resume sexual intercourse in about six weeks if you're feeling comfortable enough, with your caregiver's okay.
What will my scar be like?
At first, the scar will be slightly raised, puffy, and darker than the rest of your skin, but it'll start to shrink significantly within six weeks of surgery.
A c-section incision is only 4 to 6 inches long and about 1/8 inch wide. As the incision site continues to heal, your scar will more closely match your skin color and will narrow to about 1/16 inch wide. It might be itchy while it's healing.
C-section scars are usually very low on the abdomen. A low-lying scar will eventually be hidden by your pubic hair, probably way below the waistband of your underwear or bikini bottom.
Emotionally speaking, what should I expect?
Moms have a wide range of emotions after a c-section, so it's hard to predict how an individual will feel. You might feel disappointed if you had your heart set on a vaginal birth. Or you might not care about how you gave birth, particularly if you had complications and were worried about your baby's well-being.
Some women who end up in surgery after a long, drawn-out labor feel a sense of relief, while others are upset that they ended up with a c-section after doing all that work. And others have mixed emotions.
Some moms say they feel cheated out of a vaginal delivery, especially if they took childbirth classes and fantasized about the "ideal birth."
Others say they feel as if they're somehow less of a woman because they needed a c-section.
All of these feelings are common and may be difficult to resolve. If you feel this way, it may take some time to reconcile the reality of your birth experience with what you'd imagined during your pregnancy.
It might help to know that many women find their baby's birth, whether vaginal or c-section, very different from what they expected. If you have nagging doubts about whether the surgery was really necessary, talk to your practitioner about it and ask her to review the decision with you.
Remember that you're also likely to have the range of emotions common to most mothers during the postpartum period, regardless of how they gave birth. Postpartum blues are common, whether you had a c-section or a vaginal birth. If you're feeling really blue, seek help. You may be suffering from postpartum depression.
Finally, you may be frustrated if it seems to be taking you a long time to recover. Remember that just healing from the surgery is likely to take a significant amount of time and energy. Add to that all the postpartum changes your body is going through – along with your new round-the-clock parenting responsibilities – and you're bound to be in less-than-top condition for a while.Try to cut yourself some slack and be patient. In time, you'll be feeling better and enjoying life with your new baby.
http://www.babycenter.com/
Cesarean Delivery:
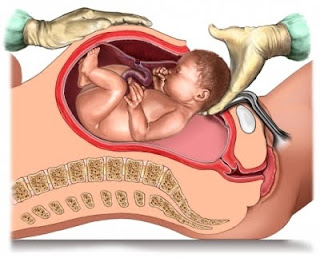
Doctor has already given advice to mom for a cesarean delivery.
Poor mom! she is scared to a great extent..i am also scared ..I have alot of things to do now..
Now the spot light is focussed directly on me..
Till this day I was safe and secured (and also hidden ;) hee hee) in my mum's protected womb ..now as the day gradually approaching I am nervous.
I will meet a whole lot of peaple as soon as I come out to this new world..first and foremost i want meet my papa who is waiting eagerly to see me..and everytime I pop upp in my mum belly he says'goblu when shall I meet you and take you in my arms?"
Not long paa..I am ready now..doctors are ready..date is given..now only matter of a few days..
Then I want to meet my grandpas and grandmas who will pamper me like anything :)
My uncle is waiting for me to come out so that he will play and give me all the toys I would love :)
It will be very hectic for me..i guess..playing all the time and also giving photo shoots with smiling faces.My uncle is all ready to take all my snaps from now itself..
But first things first..let me come out properly and securely first..then I have a lot of activities to do..
Now let us concentrate about the c-section delivery..so that mom has all the information before she proceeds for the operative procedure and can make her mind ready for the entire process..
What are my chances of having a c-section?
About 30 percent of pregnant women in the United States give birth by cesarean section these days. In certain cases the surgery is scheduled in advance. In others, it's done in response to an unforeseen complication.
Why might I need a c-section?
You may have an unplanned cesarean delivery for many reasons, such as if your cervix stops dilating, your baby stops progressing down the birth canal, or your baby's heart-rate gives your practitioner cause for concern. A planned cesarean may be recommended if:
• You've had a previous cesarean with a "classical" vertical uterine incision or more than one previous c-section. (If you've had only one previous c-section with a horizontal incision, you may be a good candidate for a vaginal birth after cesarean, or VBAC.)
• You've had some other kind of invasive uterine surgery, such as a myomectomy (the surgical removal of fibroids).
• You're carrying more than one baby. (Some twins can be delivered vaginally, but all higher-order multiples require a c-section.)
• Your baby is expected to be very large (a condition known as macrosomia).
• Your baby is in a breech (bottom first) or transverse (sideways) position. (In some cases, such as a twin pregnancy in which the first baby is head down but the second baby is breech, the breech baby may be delivered vaginally.)
• You have placenta previa (when the placenta is so low in the uterus that it covers the cervix).
• The baby has a known illness or abnormality that would make a vaginal birth risky.
• You're HIV-positive, and blood tests done near the end of pregnancy show that you have a high viral load.
What should I expect during a c-section?
Typically, your partner can be with you during the surgery. If you don't already have one, your medical team will start an IV and insert a catheter to drain urine during the procedure, and you'll be given an epidural or spinal block, which will numb the lower half of your body but leave you alert and awake. A screen will be put up so you don't have to watch the actual procedure. Once the doctor reaches the uterus and makes the final incision, she'll ease the baby out, lifting him so you get a glimpse of him before he's handed off to be cared for by a pediatrician or nurse. While the staff is examining your baby, the doctor will deliver your placenta and stitch you back up. When your baby has been examined, the pediatrician or nurse may hand him to your partner, who can hold him right next to you so you can nuzzle and kiss him while you're being stitched up. Closing your uterus and belly takes a lot longer, than opening you up. This part of the surgery usually takes about 30 minutes. When the surgery is completed, you'll be wheeled into a recovery room, where you'll be able to hold your baby and breastfeed if you want to.
Thursday, July 1, 2010
High SGPT and SGOT during pregnancy:
Every time something goes wrong somewhere in some blood test or the other for my mom and I feel guilty :(
Last time wen she met her gynae she explained that she is having some ichiness all over the body and then advised the SGPT/SGOT test for mom and they came back high..
Now what might be the reasons for that?
There are several theories as explained by practitioners for this..
Changes in metabolism during pregnancy, weight gain can cause elevated liver tests that should return to normalNormal saline flush as your body returns to pre-pregnancy state. One should exclude viral hepatitis with the appropriate blood tests. You should continue with follow-up liver tests until normal values are obtained.
There are many conditions that are commonly associated with elevations of the Liver Function Tests SGOT/AST and SGPT/ALT. There are numerous causes of having an elevation of these enzymes. SGPT/SGOT are enzymes that are associated with the function of your liver and the conversion of glucose and are usually found in the mitochondria of the liver cells. Different levels of these enzymes can indicate differing conditions and causes. These may include gallbladder disease, hepatitis, fatty liver, cirrhosis, infectious mononucleosis, alcoholism, medications and drug toxicity, CHF, heart attack, heart muscle damage, skeletal muscle injury, renal infarct, certain types of anaemia, malignancy and others. Further tests will very likely be ordered to ascertain the cause of your sister’s elevated levels. Without access to the full LFT report, there are no further details to work on or discuss.
ALT (SGPT) and AST (SGOT) are enzymes made in the liver. They are also known as transaminases. The liver uses these enzymes to metabolize amino acids and to make proteins. When liver cells are damaged or dying, ALT and AST leak into the bloodstream. Many different things can cause liver enzymes to rise above normal levels: Viral hepatitis Excessive alcohol intake/Alcoholic liver disease Liver inflammation from medications such as overdose of Acetaminophen ( Tylenol) and certain herbs, Auto-immune hepatitis - a condition where a person's immune system mistakes the liver for an invader and attacks it, Fatty liver- fat build -up in liver cells, called steatohepatitis when the fatty liver is inflammed - NASH Inherited liver diseases Liver tumors Heart failure Inflammation in the liver or gallbladder Gallstones
To help with constipation and other IBS (Irritable Bowel Syndrome) symptoms during pregnancy, some women take medications. Not all medications that may be used to treat irritable bowel syndrome are safe for pregnancy. Therefore, you should discuss medical treatment with your doctor before taking any drug. However, the following is a list of medications that are usually safe to take during pregnancy:
o Acetaminophen (IE Tylenol) - helps with pain and discomfort
o Bentyl/Dicyclomine - prevents muscles spasms in the stomach and bladder and helps to relax them. It also reduces the production of stomach acid.
o Diclectin - helps with morning sickness
o Simethicone - helps to alleviate gas in the intestinal tract.
Medications are not the only answer when it comes to helping pregnant women treat their IBS symptoms. Alternative treatments include:
o Drinking plenty of water - prevents dehydration and helps with digestion
o Regular and safe pregnancy exercises - helps aid in digestion and reduces stress
o Sufficient sleep - reduces stress
o High fiber diet - Helps move slow bowels. This includes foods such as fruit, vegetables, and high fiber cereals. Note: keep in mind that if your IBS symptoms occur because of certain fiber foods, don't include these as apart of your diet.
o Soluble fiber supplements - may help with diarrhea and constipation
o Ginger tea - Ginger tea can help treat morning sickness
o Hypnosis - This psychological treatment can be used to individually treat the symptoms a woman is experiencing.
As you can see, there are plenty of ways a pregnant woman can deal with IBS. The trick is to know what treatments work best, and incorporate them into a healthy and active lifestyle.
http://ezinearticles.com/Obstetric Cholestasis or Intrahepatic Cholestasis of Pregnancy (ICP)
What is ICP?
ICP is defined as a pregnancy-related liver condition that affects the flow of bile (a liver-produced substance that aids in the digestion and absorption of fats) to a woman’s body. This condition results in a build-up of bile acids in the blood, which in turn can lead to severe itching, and in more rare cases, jaundice.
The onset of ICP during pregnancy usually begins during the third trimester – as this is when hormone concentrations are highest – although some reports indicate it can begin as early as the first few weeks of pregnancy.
Unfortunately, the exact cause of ICP has not been determined. However, there does appear to be a genetic component to this disease; about half of all women with ICP reported having liver-related disorders in the family.
What are Intrahepatic Cholestasis of Pregnancy Symptoms?
The primary symptom of ICP is severe itching. The itching generally progresses in severity, and may develop to the point that it interferes with a woman’s daily activities, including sleep. Although the itching sensation can be present on any part of the woman’s body, it is most commonly felt on the palms of the hands or the soles of the feet.
In addition, women may experience yellowing of their skin or whites of the eyes – also known as jaundice. This is estimated to occur in about 20% of women with ICP.
How is ICP Treated?
In previous years, the primary form of medicinal treatment for ICP was a cholesterol-lowering drug called cholestyramine. However, this drug has recently been proven to be largely ineffective in lowering bile acids. In addition, a number of potentially dangerous side-effects (including vitamin K deficiency) have caused doctors to revoke this form of ICP treatment. Currently, there are several components that generally comprise treatment for ICP:
- Ursodeoxycholic Acid (Actigall): One of the most important treatments for ICP, ursodeoxycholic acid works to improve liver function by replacing toxic bile acids in the bloodstream. It has also been shown to reduce the risk of stillbirth.
- Vitamin K: Although not an essential part of ICP treatment, vitamin K therapy is sometimes recommended to combat the reduced absorption of fat-soluble vitamins that often results from having ICP. Vitamin K deficiencies are associated with increased risk for hemorrhaging in the mother and child.
- Steroids: Because pregnant women with ICP run an increased risk of pre-term labor, steroids may be administered before 32 weeks gestation to ensure the baby’s lungs are mature at birth. The drug may also reduce the itching sensation so commonly associated with ICP.
Mother and baby will also be monitored closely during the pregnancy to ensure normal fetal development is taking place. If any abnormalities are detected, early delivery may be suggested. In addition, the doctor may perform an amniocentesis test at 36 weeks gestation in order to ensure the baby’s lungs are mature enough to survive should early delivery be necessary. If this is so, labor may be induced at 36 or 37 weeks to prevent any ICP-related complications at birth.
http://www.pregnancy-info.net/obstetric_cholestasis.htmlHow is ICP diagnosed?Itching is quite often the only symptom a woman notices when she develops ICP. The itching can vary from person to person on palms of hands, arms, legs, soles of feet or all over the body. It is normally more intense at night. Due to the fact that itching is considered a normal part of pregnancy, testing for ICP is often overlooked. This can be a dangerous mistake. Any complaint of itching during pregnancy should be taken seriously and be evaluated.
Two tests should be administered to women who are experiencing pruritus which include the following:
Serum Bile Acid Test (SBA): The serum bile acid test is the most sensitive indicator of ICP. A diagnosis of ICP is often established when bile acid levels are elevated above the normal range. Since labs use differing testing methods, the normal range may fluctuate from lab to lab. The SBA test is a specialized test that should be administered after a period of fasting, as eating certain foods may increase bile production, although some labs do not make this a requirement and it often does not have a large impact on the overall results.
Standard liver enzymes include Alanine Transaminase (ALT), Aspartate Trasaminase (AST), and Alkaline Phosphotase (ALK) and are often referred to as the transaminases.
ALT is the enzyme produced within the cells of the liver. The level of ALT abnormality is increased in conditions where cells of the liver have been inflamed or undergone cell death. As the cells are damaged, the ALT leaks into the bloodstream leading to a rise in the serum levels. Any form of hepatic cell damage can result in an elevation in the ALT. The ALT level may or may not correlate with the degree of cell death or inflammation. ALT is the most sensitive marker for liver cell damage.
AST also reflects damage to the hepatic cell. It is less specific for liver disease. It may be elevated and other conditions such as a heart attack. Although AST is not a specific for liver as the ALT, ratios between ALT and AST are useful to physicians in assessing the etiology of liver enzyme abnormalities.Alkaline Phosphatase (ALK), is another liver enzyme that is evaluated during a routine LFT, but because this value is normally elevated in pregnancy, it's contribution to the diagnosis of ICP is typically disregarded by specialists.
http://www.itchymoms.com/diagnosis.html