Sunday, July 25, 2010
D-Day has come !!
Both me and Mamma are a bundle of nerves now !
Dad is busy doing the required running around the hospital and following up with my doctor aunty.
Gosh! I am both excited and scared at the same time .
I havent had much exposure to the 'external' world you know :) I was sort of getting into a comfort zone inside Mamma.
Wish me , Mamma and Daddy luck .
My next post will take sometime as I get accustomed to the external world .
I promise to share with you quite a few pics ( Dad is charging the camera as we speak :))
Goblu
Tuesday, July 6, 2010
Signs of Premature Labor:
If you start having regular contractions that cause your cervix to begin to open (dilate) or thin out (efface) before you reach 37 weeks of pregnancy, you're in preterm labor, also known as premature labor. If you deliver your baby before 37 weeks, it's called a preterm birth and your baby is considered premature.
About a quarter of all preterm births are intentional. For example, your medical team might decide to induce labor early or perform a cesarean section if you have a serious medical condition such as severe or worsening preeclampsia or if your baby has stopped growing.
The rest are known as spontaneous preterm births. You may end up having a spontaneous preterm birth if you go into labor prematurely, if your water breaks early (called preterm premature rupture of the membranes or PPROM), or if your cervix dilates prematurely with no contractions (called cervical insufficiency).
About 12 percent of babies in the United States are born prematurely. This number has gone up over the years, partly because more women are pregnant with twins or higher order multiples, who tend to arrive early.
Preterm birth can cause health problems or even be fatal for the baby if it happens too early. The more mature a child is at birth, the more likely it is that he will survive and be healthy.
Premature babies born between 34 and 37 weeks generally do very well. If you go into labor before 34 weeks, your medical team may be able to delay your labor for a few days so your baby can be given corticosteroids to help his lungs develop faster, which increases his chance of survival.
http://www.babycenter.com/
Preterm Labor Signs and Symptoms
Premature labor, also known as preterm labor, is a very serious complication of pregnancy. This is defined as labor that begins prior to 37 weeks gestation. Unfortunately, many women do not understand the signs of premature labor. Early detection can help prevent premature birth and possibly enable you to carry your pregnancy to term or to give your baby a better chance of survival.
Signs of Premature Labor
Call your practitioner if you have any of the following:
* Contractions or cramps, more than 5 in one hour
* Bright red blood from your vagina
* Pain during urination, possible urinary tract, bladder or kidney infection
* Sudden gush of clear, watery fluid from your vagina
* Low, dull backache
* Intense pelvic pressure
Prevention of Preterm Labor
While not all cases of preterm labor can be prevented there are a lot of women who will have contractions that can be prevented by simple measures.
One of the first things that your practitioner will tell you to do if you are having contractions is staying very well hydrated. We definitely see the preterm labor rates go up in the summer months. What happens with dehydration is that the blood volume decreases, therefore increasing the concentration of oxytocin (hormone that causes uterine contractions) to rise. Hydrating yourself will increase the blood volume.
Others things that you can do would be to pay attention to signs and symptoms of infections (bladder, yeast, etc.) because they can also cause infections. Keeping all of your appointments with your practitioner and calling whenever you have questions or symptoms. A lot of women are afraid of "crying wolf," but it is much better to be incorrect than to be in preterm labor and not being treated.
Management of Preterm Labor
There are a lot of variables to managing preterm labor, both in medical options and in terms of what is going on with you and/or your baby.
Here are some of the things that you may deal with when in preterm labor.
* Hydration (Oral or IV)
* Bedrest (Home or Hospital), usually left side lying
* Medications to stop labor (Magnesium sulfate, brethine, terbutaline, etc.)
* Medication to help prevent infection (More likely if your membranes have ruptured or if the contractions are caused by infection)
* Evaluation of your baby (Biophysical profile, non-stress or stress tests, amniotic fluid volume index (AFI), ultrasound, etc.)
* Medications to help your baby's lung develop more quickly (Usually if preterm birth in inevitable)
Preparation for preterm birth
The best key is always prevention and early detection. Make sure to ask your practitioner to discuss the signs and symptoms of preterm labor to you and your partner at your next visit.
http://pregnancy.about.com/od/pretermlabor/a/pretermlabor.-KJn.htm
Risk factors associated with premature labor
Some risk factors have been associated with a higher chance of premature labor. However, just because you have some risk factors does not mean that you will experience premature labor. Review the following risks factors and let your health care provider know if any apply to you.
Possible risk factor for premature labor:
- Premature labor or delivery during a previous pregnancy
- Misshapen uterus
- DES (Diethylstilbestrol) daughter (If your mother was prescribed this medication during her pregnancy to prevent miscarriage, you are considered a DES daughter. DES has been linked to shortening of the cervix.)
- Abdominal surgery during pregnancy and/or cervical cerclage (a stitch in your cervix)
- More than two second trimester miscarriages or elective abortions
- Previous Cone Biopsy or LEEP (procedures used to diagnose and/or treat the cervix of women with abnormal Pap tests)
- Carrying more than one baby
- Dehydration
- History of cervical change and/or excessive uterine contractions at less than 33 weeks in a previous pregnancy
- Serious infections with fever (greater than 101 degrees Fahrenheit) during this pregnancy
- Recurring bladder and/or kidney infections
- Excessive amount of amniotic fluid
- Unexplained vaginal bleeding after 20 weeks of pregnancy
- Using recreational drugs, such as cocaine or amphetamines
- Domestic violence
- Smoking more than 10 cigarettes per day
- Extreme emotional or physical stress
Fetal Development:34 weeks
Your amazing baby is on the move! They’ve been riding fairly high in your stretched-out womb till now (while kindly compressing your poor internal organs), but now they’re planning on making the big move to your pelvis this week. If you haven’t noticed it already, you’ll be feeling the weight shift that signals that your baby is most likely out of breech position, with their head now resting on your pubic bone. In liver news: although not quite fully formed, your little miracle’s liver is now capable of processing a certain amount of waste. In general, most of your child’s prenatal physical development is pretty much up to snuff and ready for the outside world. Naturally, further weight gain is expected—so you’re still not at maximum capacity despite probably feeling like you definitely are maxed out.
And how's mom doing?
Obviously the big change for you is the notable weight shift (known as “lightening” or “engagement”). Now that your baby is resting deeper in your pelvis, you may find yourself walking as if you're carrying a watermelon between your legs. Yes dear, you’re officially “waddling” these days. Try to comfort Now that your baby is resting deeper in your pelvis, you may find yourself walking as if you're carrying a watermelon between your legs yourself with this thought: it’s nearly over. Soon, you’ll just have to carry your adorable little watermelon in your arms. And in a rare spate of good news: this weight shift means you can breathe easier now that your lungs aren’t compressed. The not-so-good news, it’s a trade off: (we’ll wait till you’re back from the restroom) this new position has your poor bladder even more squished than before. We’d recommend writing your bladder little love poems to convince it not to leave you altogether, but unfortunately bladders don’t speak English (only Italian love poems will do).
If you've recently noticed some less-than-appealing itchy red bumps on your belly (and possibly around your thighs and belly), you've got yourself a harmless but not fun round of pruritic urticarial papules and plaques of pregnancy (PUPPP if your don't have the patience for the full name). If you feel itchy ALL over your body, that's different, and you should call your health care practitioner as this could be a liver problem.
At your next check up you can expect your physician to conduct a Group B Streptococci test (GBS), a common bacteria screening. As long as you have a strong immune system, you’re in the clear (one more reason to eat right and exercise!), but your little one is more susceptible to serious health complications (including meningitis, pneumonia and blood infection) if not diagnosed and treated properly—so the tests are good for some peace of mind. Hang in there momma, you’re already a super-star for making it this far!
http://pregnancy.baby-gaga.com/calendar
Baby
Besides looking like a newborn at 34 weeks of pregnancy, your baby is acting like a newborn as well. Her eyes open when she’s awake and close when she is sleeping. Her sleeping cycles are the same now as they will be when she is born. She has learned to blink and can see better when a bright light is shined on your stomach. She recognizes voice and sound patterns from the outside world and is most comforted by the sound of your voice.
She weighs about 4 ¾ pounds now and is about 18 inches long. Her fingernails have reached the end of her fingertips at week 34 of pregnancy and she may even scratch her face before she is born. Her fat layers are growing every week to fill up that wrinkly skin and she may have already turned into the head down position for labor.
Your baby’s central nervous system is still maturing, and her lungs are almost fully ready to breathe air. If your baby is born this week, she has a 99% chance of survival outside of the womb, pretty darn good odds.
Mom
The last few weeks can be uncomfortable and tiring. The weight of your baby and your body may start to leave you feeling fatigued at week 34 of pregnancy. Be sure to rest up and save some energy for the big day. In the next couple of weeks, you will most likely be tested for Group B streptococcus (GBS). GBS is a type of bacteria that some pregnant women carry in their vaginal or rectal areas. This bacteria is harmless to you, but can be transmitted to your baby during childbirth and cause some complications like meningitis, bacterial blood infections, and pneumonia. If you test positive for GBS, your doctor can prevent many of these complications by administering an antibiotic to you through IV during labor.
As you get closer to your labor day, have you thought about how this baby will affect your relationship? If this is your first baby, a new member to the family can be exciting, but overwhelming. If you are married or living with your partner, having that first baby can strengthen your relationship greatly. On the other hand, if you have already had some differences, a baby can add even more stress. The key to a great relationship with your partner is good communication.
What often happens with first babies is that one parent is more ready and willing to quickly transition their lifestyle than the other. Add to that the stress of decreased sex, little sleep, and a high maintenance baby that takes all of your energy and focus. It’s no wonder that relationships can be a bit strained that first year.
Be proactive and make a commitment to your partner. Commit to weekly or at least monthly dates with just the two of you, no baby. If you are low on cash, a picnic or a hike will do fine. OR take baby to a babysitter and cook yourselves a romantic dinner.
When conflicts arise, talk them out before resentments show. Try and get your partner involved with the baby as much as possible. If you are nursing, let dad bathe the baby. Anyway you can get him to bond to baby will help him bond with the family lifestyle. Remember that bonding is harder for dad at first; he didn’t carry your child for nine months, he’s not able to nurse, and babies naturally bond to mom first.
Encourage your partner’s dad skills by encouraging him to participate more. While your baby’s first year can be a challenge, with hard work and dedication, you will discover more love than you have ever known, from your partner and your child.
http://smartmomma.com/pregnancy/
Week 34 Pregnancy Symptoms
Flatulence: As your third trimester progresses, you may be getting gassier. Anxiety just makes those gassy feelings worse — you tend to swallow more air when you’re stressed — so try this tension tamer: Breathe deeply through your nose and out through your mouth for a minute or two each day.
Constipation: Need to rev up those slow-moving bowels? Rough up your diet with some dried fruits, fruits and veggies, and whole grains. One thing you don’t want to do — take laxatives (even herbal ones). Get your practitioner on board before taking any medicine for constipation.
Increased vaginal discharge: As your pregnancy progresses, you could see an increase in vaginal discharge. Blame pregnancy hormones (especially estrogen) for this symptom — they increase blood flow to the pelvic area and stimulate the mucous membranes (making your juices flow). Wearing undies with a cotton crotch can keep you drier (and that can curb odors).
Hemorrhoids: Constipation’s almost constant sidekick? Hemorrhoids. These pesky piles can be kept to a minimum by doing Kegels, which can improve circulation to the area.
Backaches: Your shifting center of gravity from back to belly puts more pressure and (ouch!) pain on your lower back. There are many solutions to cure your aching back, so if one doesn’t work, another most certainly will. One to try: Take a break and stretch, stand, or walk. Sitting too long can make your back hurt even more.
Leg cramps: Leg cramps are most common around now, when the three main culprits — pregnancy weight, swelling, and fatigue — are at their peak. If you feel a spasm, try standing on a cold surface (that can sometimes stop one).
Stretch marks: If you’re fair-haired and have a genetic predisposition toward stretch marks, you’re more likely to get them than someone who’s darker-haired (or skinned). But no matter what your skin or hair color, you can try to keep these classic marks of maternity to a minimum by keeping your weight gain slow and steady.
Mild swelling of ankles and feet: As you get bigger and your body tissues accumulate and retain fluids, you may experience swelling in your ankles, feet, and fingers. Slipping into comfy slippers at the end of the workday can help soothe your swollen tootsies.
Hair changes: You knew your hair would grow faster and more lustrous while you were pregnant, but you probably didn’t expect it to grow in places you weren’t expecting — like your cheeks, chin, and back. Waxing is safe during pregnancy; but since skin is extra-sensitive now, ask for a formula for sensitive skin.
Shortness of breath: As your pregnant belly gets bigger, your lungs won’t be able to expand as fully, so you may feel winded, even after a trip to the bathroom. Sleeping propped on your left side can help at night, and just take it easy.
Difficulty sleeping: If you’re not worrying about your impending D-day, then leg cramps and trips to bathroom are banishing any chance of shut-eye. Try lulling yourself to sleep with a warm bath and a cup of warm milk and read a book or listen to music instead of surfing the net or watching TV (those activities can keep you up).
Leaking colostrum: As your due date approaches and the third trimester wears on, your breasts may leak colostrum — yellowish pre-milk that will be your baby’s first drink. You won’t be leaking more than a few drops, but if you feel uncomfortable, try nursing pads.
http://www.whattoexpect.com/pregnancy/week-by-week/Fetal Development:33 weeks
- The baby is now 4.4 pounds (2 kg) and around 17.5 inches (44cm) in length.
- The diameter of the head is about 8.5cm.
- The baby fuzz, lanugo, is disappearing.
- Your baby drinks about a pint of amniotic fluid a day.
- You may gain a pound a week (500g) for the rest of your pregnancy.
- Half of your weight gain will go directly to your baby.
You may gain a pound a week for the rest of your pregnancy. Do not stop eating or start skipping meals as your weight increases. Both you and your baby need the calories and nutrition you receive from a healthy diet. Calcium intake is extremely important during pregnancy because the baby will draw calcium from the mother to make and harden bone. This can greatly weaken her own bones and teeth because the developing fetus will take minerals from the mother's skeletal structure as needed.
http://www.baby2see.com/development
Fetal development in pregnancy week 33:
For all the weight and bulk you’re lugging around these days, you’d think your little champ should weigh much more than a mere 5 lbs and measly 17 inches in height, but nope, that’s about the average size for a baby in its thirty-third week. In terms of appearances, they’re getting cuter and pudgier every minute as they pile on the baby fat for those adorable little wrist rolls and chubby toes. And as we’re sure you’ve already noticed they’re getting stronger with every passing day. Nowadays, it’s possible to observe a well-placed kick just by watching your belly—but you already knew that didn’t you? Although they’re getting stronger, your bigger-by-the-day baby is losing space to move around, so the actual rate of movement will drop off in the last few weeks, despite that powerful drop-kick they’ve been working on. Hey, did you know you’ll continue feeling their movements even during labor?
And how's mom doing?
Here’s a good way to deal with your mounting impatience: map out your plan of action for the big day. It’s an important and necessary step that’s also pretty soothing and fun. So, get out a piece of paper and pen. If you think about it, planning all the details now can be a real saving grace once Massaging the perineum (the area around the vagina) can reduce your chance of it tearing during delivery the chaos and pain of labor starts up. This would include having a packed bag with a change of comfortable clothes, reading material, maybe an i-pod and your camera or camcorder (whichever you decide, if any at all). Know your driving route to the health center. Or if you’re delivering at home, make sure you have the delivery room prepared (equipped with your most favorite soothing music), and all necessary instruments and materials ready for use. Of course, get your doctor or midwife on speed-dial. Massaging the perineum (the area around the vagina) can reduce your chance of it tearing during delivery and there’s no time like the present to start. Be on your toes (not literally, just mentally) as it's now totally conceivable you might have to spring into action any day! Then again, it might still be another seven weeks.
http://pregnancy.baby-gaga.com/calendar/week33
Friday, July 2, 2010
Recovering from a cesarean delivery:
Like any new mother, you'll probably feel both euphoric about and overwhelmed by the new person in your arms. But you'll also be recovering from major abdominal surgery while dealing with typical postpartum issues such as engorged breasts, mood swings, and vaginal discharge.
C-section patients typically stay just three or four days in the hospital before going home. But your recovery will be measured in weeks, not days, so once home you'll need help taking care of yourself and your new baby. What's more, if you have other children, they may be feeling needy after you've been away from them for a few days, to say nothing of the fact that you're returning home with a new baby! Plan to get all the help you can.
What will I get for postpartum pain relief?
If you have an epidural or spinal for your c-section, your anesthesiologist may add morphine, which can provide excellent postpartum pain relief for up to 24 hours without the grogginess that you get from systemic narcotics. Some anesthesiologists leave the epidural in for 12 to 24 hours after surgery so you can get more medication through it if needed.
Once your regional analgesia is no longer providing adequate pain relief, you'll be given systemic pain medication, usually pills containing a narcotic and possibly acetaminophen. It may help to take ibuprofen, too. You'll also be given a stool softener to counteract the constipating effect of the narcotic.
If you have general anesthesia for your surgery or you don't get a dose of morphine through your spinal or epidural afterward, you'll be given systemic narcotics for immediate postpartum pain relief. You'll either get a shot of pain medication every three to four hours or you'll use a system called "patient-controlled analgesia": You push a button when you're feeling discomfort that delivers medication through your IV. A machine controls the doses so you don't get more than what's safe.
In any case, don't be shy about asking your nurse for more medication if you're uncomfortable. You don't need to suffer in silence, and the longer you wait to ask for the medication you need, the harder it is to control pain in the end.
If the medication that's been ordered for you isn't covering your pain, let your nurse know. If the nurse can't help you, ask to see an obstetrician or anesthesiologist. The more comfortable you are, the easier it'll be to breastfeed your baby and to get moving again.
What's recovery like during the first few days?
You may feel groggy and possibly nauseated right after surgery. Nausea can last up to 48 hours, but your caregiver can give you medication to minimize your discomfort. Many moms also feel itchy all over, particularly those who received narcotics in their epidural or spinal. If this happens to you, let your caregiver know so she can give you medication to relieve the itchiness.
If you plan to breastfeed, you can start in the recovery room right after surgery. Ask the nurse to show you how to nurse in the side-lying position or using the football hold, so there won't be pressure on your incision.
Breastfeeding can be challenging in the days after a c-section because of the pain from a healing incision. Ask to see a lactation consultant as soon as possible to help you position your baby comfortably so you don't end up with sore nipples. If the hospital doesn't have a lactation consultant, ask for the nurse who's the resident expert.
You may feel numbness and soreness at the incision site, and the scar will be slightly raised, puffy, and darker than your natural skin tone.
Your doctor will come by daily to see how you're doing and check that the wound is healing properly.
Anything that puts pressure on the abdominal area will probably be painful at first, but you'll feel a bit better day-by-day. Be sure to use your hands or a pillow to support your incision when you cough, sneeze, or laugh.
Your nurse will come by every few hours at first to check on you and help you. She'll take your vital signs, feel your belly to make sure your uterus is firm, and assess the amount of vaginal bleeding. Like any woman who just delivered a baby, you'll have a vaginal discharge called lochia, which consists of blood and sloughed-off tissue from the lining of your uterus. For the first three or four days, it will be bright red.
Your nurse will also instruct you on how to cough or do breathing exercises to expand your lungs and clear them of any accumulated fluid, which is particularly important if you've had general anesthesia. This will reduce the risk of pneumonia.
If everything's okay, your nurse will remove your IV and urinary catheter, usually within 12 hours of surgery, and you'll likely be able to start eating bland, mild foods if you feel like it.
You might have some gas pain and bloating during the first two days. Gas tends to build up because the intestines are sluggish after surgery.
Getting up and moving around will help your digestive system get going again.
If you're in great discomfort, the nurse may give you some over-the-counter medication that contains simethicone, a substance that allows gas bubbles to come together more easily, making the gas easier to expel. Simethicone is safe to take while breastfeeding.
You may be encouraged to get out of bed the day of surgery and certainly by the next day. (Do not, however, attempt to get up by yourself.
The nurse should be at your side the first time.) In the meantime, get the blood going in your legs by wiggling your feet, rotating your ankles, and moving and stretching your legs.
Just walking to the bathroom may seem impossible at first, but moving around is important for your recovery. It will help your circulation and make it much less likely that you'll develop blood clots. What's more, it will make your bowels less sluggish, which will help you feel a whole lot more comfortable sooner.
It's also important to get to the bathroom to urinate regularly. A full bladder makes it harder for the uterus to stay contracted and increases pressure on the wound.
By the second day, you should be taking a couple of short walks with help from your partner or a nurse. Try to take your walks a short time after you've taken pain medication, when you're likely to feel more comfortable.
In three to four days, your doctor will probably remove your sutures or staples. This takes just minutes, and you may feel a small pinch but no pain. After that, if all's well, you'll be sent home.
What's recovery like after I leave the hospital?
Expect to need help – and lots of it – once you get home. If nobody offers, ask for support from your partner, parents, in-laws, and friends.
If you're worried that you may not have enough support, hire paid help if you can afford it.
You'll likely be given a prescription for more painkillers and a stool softener before you leave the hospital. You may need prescription painkillers for up to a week after surgery, gradually transitioning to over-the-counter pain relievers. (If you're breastfeeding, don't take aspirin or drugs containing acetylsalicylic acid.)
Drink plenty of fluids to help you avoid constipation. Your incision will likely feel better day-by-day, quite noticeably so after several days, though it may continue to be tender for several weeks.
Call your caregiver if you have signs of an infection, including:
* warmth, redness, or swelling at the incision site
* oozing from the incision site; worsening or sudden onset of pain
* any fever (even if your incision looks fine)
Your vaginal bleeding and discharge should be diminishing, though it may last up to six weeks. It should gradually turn from bright red to pink and then yellow-white. If menstrual-type bleeding continues past the first four days after delivery or comes back after slowing, call your healthcare provider.
For more information on warning signs of a medical problem in the weeks after delivery, see our article on when to call your practitioner.
How active should I expect to be?
While it's essential to get plenty of rest once you're home, you also need to get up and walk around regularly. Walking promotes healing and helps prevent complications such as blood clots. But don't overdo it.
Start slowly and increase your activity gradually. Since you're recovering from major abdominal surgery, your belly will feel sore for some time. Take it easy and avoid heavy household work or lifting anything heavier than your baby for eight weeks.
In six to eight weeks, you'll be able to start exercising moderately – but wait until your caregiver gives you the go-ahead. It may be several months before you're back to your former fit self. You'll be able to resume sexual intercourse in about six weeks if you're feeling comfortable enough, with your caregiver's okay.
What will my scar be like?
At first, the scar will be slightly raised, puffy, and darker than the rest of your skin, but it'll start to shrink significantly within six weeks of surgery.
A c-section incision is only 4 to 6 inches long and about 1/8 inch wide. As the incision site continues to heal, your scar will more closely match your skin color and will narrow to about 1/16 inch wide. It might be itchy while it's healing.
C-section scars are usually very low on the abdomen. A low-lying scar will eventually be hidden by your pubic hair, probably way below the waistband of your underwear or bikini bottom.
Emotionally speaking, what should I expect?
Moms have a wide range of emotions after a c-section, so it's hard to predict how an individual will feel. You might feel disappointed if you had your heart set on a vaginal birth. Or you might not care about how you gave birth, particularly if you had complications and were worried about your baby's well-being.
Some women who end up in surgery after a long, drawn-out labor feel a sense of relief, while others are upset that they ended up with a c-section after doing all that work. And others have mixed emotions.
Some moms say they feel cheated out of a vaginal delivery, especially if they took childbirth classes and fantasized about the "ideal birth."
Others say they feel as if they're somehow less of a woman because they needed a c-section.
All of these feelings are common and may be difficult to resolve. If you feel this way, it may take some time to reconcile the reality of your birth experience with what you'd imagined during your pregnancy.
It might help to know that many women find their baby's birth, whether vaginal or c-section, very different from what they expected. If you have nagging doubts about whether the surgery was really necessary, talk to your practitioner about it and ask her to review the decision with you.
Remember that you're also likely to have the range of emotions common to most mothers during the postpartum period, regardless of how they gave birth. Postpartum blues are common, whether you had a c-section or a vaginal birth. If you're feeling really blue, seek help. You may be suffering from postpartum depression.
Finally, you may be frustrated if it seems to be taking you a long time to recover. Remember that just healing from the surgery is likely to take a significant amount of time and energy. Add to that all the postpartum changes your body is going through – along with your new round-the-clock parenting responsibilities – and you're bound to be in less-than-top condition for a while.Try to cut yourself some slack and be patient. In time, you'll be feeling better and enjoying life with your new baby.
http://www.babycenter.com/
Cesarean Delivery:
Doctor has already given advice to mom for a cesarean delivery.
Poor mom! she is scared to a great extent..i am also scared ..I have alot of things to do now..
Now the spot light is focussed directly on me..
Till this day I was safe and secured (and also hidden ;) hee hee) in my mum's protected womb ..now as the day gradually approaching I am nervous.
I will meet a whole lot of peaple as soon as I come out to this new world..first and foremost i want meet my papa who is waiting eagerly to see me..and everytime I pop upp in my mum belly he says'goblu when shall I meet you and take you in my arms?"
Not long paa..I am ready now..doctors are ready..date is given..now only matter of a few days..
Then I want to meet my grandpas and grandmas who will pamper me like anything :)
My uncle is waiting for me to come out so that he will play and give me all the toys I would love :)
It will be very hectic for me..i guess..playing all the time and also giving photo shoots with smiling faces.My uncle is all ready to take all my snaps from now itself..
But first things first..let me come out properly and securely first..then I have a lot of activities to do..
Now let us concentrate about the c-section delivery..so that mom has all the information before she proceeds for the operative procedure and can make her mind ready for the entire process..
What are my chances of having a c-section?
About 30 percent of pregnant women in the United States give birth by cesarean section these days. In certain cases the surgery is scheduled in advance. In others, it's done in response to an unforeseen complication.
Why might I need a c-section?
You may have an unplanned cesarean delivery for many reasons, such as if your cervix stops dilating, your baby stops progressing down the birth canal, or your baby's heart-rate gives your practitioner cause for concern. A planned cesarean may be recommended if:
• You've had a previous cesarean with a "classical" vertical uterine incision or more than one previous c-section. (If you've had only one previous c-section with a horizontal incision, you may be a good candidate for a vaginal birth after cesarean, or VBAC.)
• You've had some other kind of invasive uterine surgery, such as a myomectomy (the surgical removal of fibroids).
• You're carrying more than one baby. (Some twins can be delivered vaginally, but all higher-order multiples require a c-section.)
• Your baby is expected to be very large (a condition known as macrosomia).
• Your baby is in a breech (bottom first) or transverse (sideways) position. (In some cases, such as a twin pregnancy in which the first baby is head down but the second baby is breech, the breech baby may be delivered vaginally.)
• You have placenta previa (when the placenta is so low in the uterus that it covers the cervix).
• The baby has a known illness or abnormality that would make a vaginal birth risky.
• You're HIV-positive, and blood tests done near the end of pregnancy show that you have a high viral load.
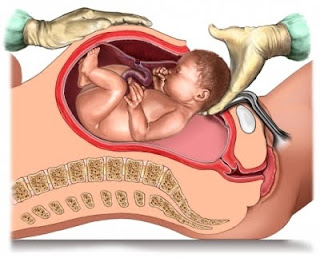
What should I expect during a c-section?
Typically, your partner can be with you during the surgery. If you don't already have one, your medical team will start an IV and insert a catheter to drain urine during the procedure, and you'll be given an epidural or spinal block, which will numb the lower half of your body but leave you alert and awake. A screen will be put up so you don't have to watch the actual procedure. Once the doctor reaches the uterus and makes the final incision, she'll ease the baby out, lifting him so you get a glimpse of him before he's handed off to be cared for by a pediatrician or nurse. While the staff is examining your baby, the doctor will deliver your placenta and stitch you back up. When your baby has been examined, the pediatrician or nurse may hand him to your partner, who can hold him right next to you so you can nuzzle and kiss him while you're being stitched up. Closing your uterus and belly takes a lot longer, than opening you up. This part of the surgery usually takes about 30 minutes. When the surgery is completed, you'll be wheeled into a recovery room, where you'll be able to hold your baby and breastfeed if you want to.
Thursday, July 1, 2010
High SGPT and SGOT during pregnancy:
Every time something goes wrong somewhere in some blood test or the other for my mom and I feel guilty :(
Last time wen she met her gynae she explained that she is having some ichiness all over the body and then advised the SGPT/SGOT test for mom and they came back high..
Now what might be the reasons for that?
There are several theories as explained by practitioners for this..
Changes in metabolism during pregnancy, weight gain can cause elevated liver tests that should return to normalNormal saline flush as your body returns to pre-pregnancy state. One should exclude viral hepatitis with the appropriate blood tests. You should continue with follow-up liver tests until normal values are obtained.
There are many conditions that are commonly associated with elevations of the Liver Function Tests SGOT/AST and SGPT/ALT. There are numerous causes of having an elevation of these enzymes. SGPT/SGOT are enzymes that are associated with the function of your liver and the conversion of glucose and are usually found in the mitochondria of the liver cells. Different levels of these enzymes can indicate differing conditions and causes. These may include gallbladder disease, hepatitis, fatty liver, cirrhosis, infectious mononucleosis, alcoholism, medications and drug toxicity, CHF, heart attack, heart muscle damage, skeletal muscle injury, renal infarct, certain types of anaemia, malignancy and others. Further tests will very likely be ordered to ascertain the cause of your sister’s elevated levels. Without access to the full LFT report, there are no further details to work on or discuss.
ALT (SGPT) and AST (SGOT) are enzymes made in the liver. They are also known as transaminases. The liver uses these enzymes to metabolize amino acids and to make proteins. When liver cells are damaged or dying, ALT and AST leak into the bloodstream. Many different things can cause liver enzymes to rise above normal levels: Viral hepatitis Excessive alcohol intake/Alcoholic liver disease Liver inflammation from medications such as overdose of Acetaminophen ( Tylenol) and certain herbs, Auto-immune hepatitis - a condition where a person's immune system mistakes the liver for an invader and attacks it, Fatty liver- fat build -up in liver cells, called steatohepatitis when the fatty liver is inflammed - NASH Inherited liver diseases Liver tumors Heart failure Inflammation in the liver or gallbladder Gallstones
To help with constipation and other IBS (Irritable Bowel Syndrome) symptoms during pregnancy, some women take medications. Not all medications that may be used to treat irritable bowel syndrome are safe for pregnancy. Therefore, you should discuss medical treatment with your doctor before taking any drug. However, the following is a list of medications that are usually safe to take during pregnancy:
o Acetaminophen (IE Tylenol) - helps with pain and discomfort
o Bentyl/Dicyclomine - prevents muscles spasms in the stomach and bladder and helps to relax them. It also reduces the production of stomach acid.
o Diclectin - helps with morning sickness
o Simethicone - helps to alleviate gas in the intestinal tract.
Medications are not the only answer when it comes to helping pregnant women treat their IBS symptoms. Alternative treatments include:
o Drinking plenty of water - prevents dehydration and helps with digestion
o Regular and safe pregnancy exercises - helps aid in digestion and reduces stress
o Sufficient sleep - reduces stress
o High fiber diet - Helps move slow bowels. This includes foods such as fruit, vegetables, and high fiber cereals. Note: keep in mind that if your IBS symptoms occur because of certain fiber foods, don't include these as apart of your diet.
o Soluble fiber supplements - may help with diarrhea and constipation
o Ginger tea - Ginger tea can help treat morning sickness
o Hypnosis - This psychological treatment can be used to individually treat the symptoms a woman is experiencing.
As you can see, there are plenty of ways a pregnant woman can deal with IBS. The trick is to know what treatments work best, and incorporate them into a healthy and active lifestyle.
http://ezinearticles.com/Obstetric Cholestasis or Intrahepatic Cholestasis of Pregnancy (ICP)
What is ICP?
ICP is defined as a pregnancy-related liver condition that affects the flow of bile (a liver-produced substance that aids in the digestion and absorption of fats) to a woman’s body. This condition results in a build-up of bile acids in the blood, which in turn can lead to severe itching, and in more rare cases, jaundice.
The onset of ICP during pregnancy usually begins during the third trimester – as this is when hormone concentrations are highest – although some reports indicate it can begin as early as the first few weeks of pregnancy.
Unfortunately, the exact cause of ICP has not been determined. However, there does appear to be a genetic component to this disease; about half of all women with ICP reported having liver-related disorders in the family.
What are Intrahepatic Cholestasis of Pregnancy Symptoms?
The primary symptom of ICP is severe itching. The itching generally progresses in severity, and may develop to the point that it interferes with a woman’s daily activities, including sleep. Although the itching sensation can be present on any part of the woman’s body, it is most commonly felt on the palms of the hands or the soles of the feet.
In addition, women may experience yellowing of their skin or whites of the eyes – also known as jaundice. This is estimated to occur in about 20% of women with ICP.
How is ICP Treated?
In previous years, the primary form of medicinal treatment for ICP was a cholesterol-lowering drug called cholestyramine. However, this drug has recently been proven to be largely ineffective in lowering bile acids. In addition, a number of potentially dangerous side-effects (including vitamin K deficiency) have caused doctors to revoke this form of ICP treatment. Currently, there are several components that generally comprise treatment for ICP:
- Ursodeoxycholic Acid (Actigall): One of the most important treatments for ICP, ursodeoxycholic acid works to improve liver function by replacing toxic bile acids in the bloodstream. It has also been shown to reduce the risk of stillbirth.
- Vitamin K: Although not an essential part of ICP treatment, vitamin K therapy is sometimes recommended to combat the reduced absorption of fat-soluble vitamins that often results from having ICP. Vitamin K deficiencies are associated with increased risk for hemorrhaging in the mother and child.
- Steroids: Because pregnant women with ICP run an increased risk of pre-term labor, steroids may be administered before 32 weeks gestation to ensure the baby’s lungs are mature at birth. The drug may also reduce the itching sensation so commonly associated with ICP.
Mother and baby will also be monitored closely during the pregnancy to ensure normal fetal development is taking place. If any abnormalities are detected, early delivery may be suggested. In addition, the doctor may perform an amniocentesis test at 36 weeks gestation in order to ensure the baby’s lungs are mature enough to survive should early delivery be necessary. If this is so, labor may be induced at 36 or 37 weeks to prevent any ICP-related complications at birth.
http://www.pregnancy-info.net/obstetric_cholestasis.htmlHow is ICP diagnosed?Itching is quite often the only symptom a woman notices when she develops ICP. The itching can vary from person to person on palms of hands, arms, legs, soles of feet or all over the body. It is normally more intense at night. Due to the fact that itching is considered a normal part of pregnancy, testing for ICP is often overlooked. This can be a dangerous mistake. Any complaint of itching during pregnancy should be taken seriously and be evaluated.
Two tests should be administered to women who are experiencing pruritus which include the following:
Serum Bile Acid Test (SBA): The serum bile acid test is the most sensitive indicator of ICP. A diagnosis of ICP is often established when bile acid levels are elevated above the normal range. Since labs use differing testing methods, the normal range may fluctuate from lab to lab. The SBA test is a specialized test that should be administered after a period of fasting, as eating certain foods may increase bile production, although some labs do not make this a requirement and it often does not have a large impact on the overall results.
Standard liver enzymes include Alanine Transaminase (ALT), Aspartate Trasaminase (AST), and Alkaline Phosphotase (ALK) and are often referred to as the transaminases.
ALT is the enzyme produced within the cells of the liver. The level of ALT abnormality is increased in conditions where cells of the liver have been inflamed or undergone cell death. As the cells are damaged, the ALT leaks into the bloodstream leading to a rise in the serum levels. Any form of hepatic cell damage can result in an elevation in the ALT. The ALT level may or may not correlate with the degree of cell death or inflammation. ALT is the most sensitive marker for liver cell damage.
AST also reflects damage to the hepatic cell. It is less specific for liver disease. It may be elevated and other conditions such as a heart attack. Although AST is not a specific for liver as the ALT, ratios between ALT and AST are useful to physicians in assessing the etiology of liver enzyme abnormalities.Alkaline Phosphatase (ALK), is another liver enzyme that is evaluated during a routine LFT, but because this value is normally elevated in pregnancy, it's contribution to the diagnosis of ICP is typically disregarded by specialists.
http://www.itchymoms.com/diagnosis.html
Friday, June 25, 2010
Normal newborn size:
I think it is..otherwise why and my mom would discuss every time when they meet about my size that is expected I am born!
When mom started searching the net there were so many information available about new born size and how they should weigh when they come out on their mom's lap..
The newborn size:
In their first year, newborns grow a big way, with most tripling their birth weight and increasing their length by about 50%.
From your baby's first day, health care providers will keep track of weight, length, and head size. Growth is a good indicator of general health, and babies who are progressing well are generally healthy, while poor growth can be a sign of a problem.
What Newborns Weigh
Just like adults, newborns come in a range of healthy sizes. Most full-term babies (born between 37 and 40 weeks) weigh somewhere between 6 pounds, 2 ounces (2,812 grams) and 9 pounds, 2 ounces (4,173 grams). Their average length ranges from 19 to 21 inches (48 to 53 centimeters).
A newborn who is lighter or heavier than the average range is probably perfectly fine but might receive extra attention from the doctors and nurses after delivery just to make sure there are no problems.
A number of things can affect a baby's size at birth. The length of the pregnancy is important. Babies born at their due date or later tend to be larger than those born earlier. Babies born prematurely are often smaller than full-term babies.
Other factors include:
* Size of parents. Tall parents may have larger-than-average newborns; short parents may have smaller-than-average newborns.
* Multiple births. If you're having twins, triplets, or more, you can count on your babies being relatively small. Multiples not only have to share their growing space in the uterus, they also are often born early, which leads to small size at birth.
* Birth order. First babies are sometimes smaller than brothers or sisters born later.
* Gender. Girls tend to be smaller, boys larger, but the differences are slight at birth.
* Mother's health during pregnancy. Factors that can lead to a lower birth weight include a mother's high blood pressure, heart problems, or use of cigarettes, alcohol, or illegal drugs during the pregnancy. If the mother has diabetes, the baby may have a higher birth weight. All conditions that can affect a baby's weight should be closely monitored by the mother's doctor. In addition, women should not smoke, drink alcohol, or use illegal drugs during pregnancy.
* Nutrition during pregnancy. Proper nutrition is essential for a baby's growth in the uterus and beyond. A poor diet during pregnancy can affect how much a newborn weighs and how the infant grows.
* Baby's health. Medical problems, including some birth defects and certain infections acquired during the pregnancy, can affect a child's birth weight and later growth.
Growth and Premature Babies
Premature babies generally are smaller and lighter than other newborns. A preemie's weight will be largely determined by how early he or she was born. The time the infant has missed being in the womb was growing time, so the baby has to do that growing in the outside world.
Many pre-term babies are classified as having "low birth weight" or "very low birth weight." In medical terms, "low birth weight" means a baby weighs less than 5 pounds, 8 ounces (2,630 grams) at birth. That's the case for about 1 in every 13 babies in the United States, so it's quite common. "Very low birth weight" means a baby weighs less than 3 pounds, 5 ounces (1,587 grams). Most babies with low or very low birth weight were born prematurely.
Premature babies are given special medical attention immediately after birth, and a pediatric specialist called a neonatologist may be involved in their care. Many premature babies spend time in the neonatal intensive care unit (NICU) while they receive medical care, including feeding and observation of growth.
Is Bigger Better?
In the old days, a "strapping" baby with chubby cheeks and dimpled thighs was many people's picture of a healthy newborn. But a baby born much larger than average may have special medical problems that need attention. Some exceptionally large babies, especially those born to mothers with diabetes, including gestational diabetes, may have problems for a few days keeping blood sugar levels up and may require extra feedings, or even intravenous glucose, to prevent those levels from falling too low.
How Newborns Grow
Babies are born with some extra fluid, so it is perfectly normal for a newborn to drop a few ounces when that fluid is lost in the first few days of life. A healthy newborn is expected to lose 7% to 10% of the birth weight but should regain that weight by about 2 weeks after birth.
During their first month, most newborns continue to gain weight at a rate of at least 5 ounces (141 grams) a week. They generally grow in height about 1 to 1.5 inches (2.54 to 3.81 centimeters) during the first month. Many newborns go through a period of rapid growth when they are 7 to 10 days old and again at 3 and 6 weeks.
Should I Be Concerned?
Newborns are so small, and it can be hard to know if your baby is gaining weight the way he or she should. You may worry that your baby has lost too much weight in the first few days or isn't taking enough breast milk or formula. Most likely, everything is fine. But if you are concerned at all, check with your doctor.
What's Next?
Being small or large at birth doesn't necessarily mean a baby will be small or large later in childhood or as an adult. Plenty of towering teenagers began life as small babies, and the biggest baby on the block can grow up to be a petite adult.
By the time they're adults, kids tend to resemble their parents in size. Genetics, as well as good nutrition and your attention, will play a large part in determining how your baby grows in the years to come.
Whether your baby starts out large, small, or in between, in the next few months you can expect your infant to keep growing fast.
http://kidshealth.org/parent/growth/
The Normal Newborn
The average duration of pregnancy is 40 weeks. A baby born after this period weighs 2.8 kg. ( on an average ).
Any newborn with a birth weight of < 2.5 kg. is classified as a Low Birth Weight Baby and needs special care.
Following are the characteristics of a normal newborn baby:
* Weight 2.5 – 3.5 kg.
* Length 50 cm.
* Head circumference 35 cm.
* Heart rate 120 – 140 per minute.
* Respiratory rates 30 – 40 per minute.
The normal baby may be slightly bluish in the extremities a short while after birth but becomes pink within a few hours.
Urine is passed during birth or immediately after birth, but a vast majority passes urine within the 24 hours.
The first stool, which the baby passes, is known as meconium, it is black in color and is paste like. Meconium is passes within the first day and the stools change to golden brown over the next 2 – 3 days.
The infant is normally ready for the feed within 3 – 4 hours after birth and where ever possible should be put to the mother’s breast.
http://health.indiamart.com/kidshealth/newborn/
Monday, June 21, 2010
Baby's position:
I have heard there are different orientations of a baby possible and depending on that they are named differently.
Normal Position Of The Baby
Normal Fetal Position
 The term "fetal presentation" refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.
The term "fetal presentation" refers to the part of your baby's body that is closest to the birth canal. In most full-term pregnancies, the baby is positioned head down, or cephalic, in the uterus.Breech Presentation
 If your baby is breech, his bottom is the part of his body closest to the birth canal. No one is sure what causes a breech presentation, but it happens in 3% to 5% of single-baby deliveries.
If your baby is breech, his bottom is the part of his body closest to the birth canal. No one is sure what causes a breech presentation, but it happens in 3% to 5% of single-baby deliveries.As your pregnancy nears full term, your caregiver will check your baby's position during regular prenatal visits. Common methods for assessing fetal position include vaginal exams, feeling your abdomen, and listening to the baby's heartbeat with a Doppler device.
Types Of Breech Presentation
 There are three types of breech presentation: complete, incomplete, and frank.
There are three types of breech presentation: complete, incomplete, and frank.Complete breech is when both of the baby's knees are bent and his feet and bottom are closest to the birth canal.
Incomplete breech is when one of the baby's knees is bent and his foot and bottom are closest to the birth canal.
Frank breech is when the baby's legs are folded flat up against his head and his bottom is closest to the birth canal.
Complications of Breech
Prolapsed Umbilical Cord
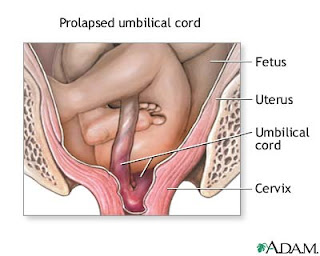 A prolapsed umbilical cord is common in breech deliveries. This happens when part of the umbilical cord slips down through the cervix before the baby does. The cord is then compressed during contractions, which cuts down on blood flow to the baby. An emergency cesarean section is usually needed.
A prolapsed umbilical cord is common in breech deliveries. This happens when part of the umbilical cord slips down through the cervix before the baby does. The cord is then compressed during contractions, which cuts down on blood flow to the baby. An emergency cesarean section is usually needed.Correcting Breech
External Version
 If you're near term and your baby is breech, your doctor may try to manually move him into a head-down position for delivery. There are two ways to do this: During an external version, the doctor moves your baby by pressing on the outside of your belly. During an internal version, the doctor inserts his hand through your vagina and cervix and moves the baby from the inside.
If you're near term and your baby is breech, your doctor may try to manually move him into a head-down position for delivery. There are two ways to do this: During an external version, the doctor moves your baby by pressing on the outside of your belly. During an internal version, the doctor inserts his hand through your vagina and cervix and moves the baby from the inside.If your doctor can't manually reposition your baby, a cesarean section may be needed.
Other Presentations
Posterior Presentation
 If your baby is in a posterior position, his face is turned up toward your belly. This can make labor longer and more difficult, since the widest part of his head has to fit through the birth canal.
If your baby is in a posterior position, his face is turned up toward your belly. This can make labor longer and more difficult, since the widest part of his head has to fit through the birth canal.You may be able to help your baby rotate into a normal, face-down position by getting on all fours with your bottom in the air, which allows your uterus to drop forward. Your doctor may also try to reposition your baby by reaching in through your vagina and gently rotating his head with his hand or forceps. If none of these methods works, a cesarean section may be needed.
Other Presentations
Transverse Lie
 If your baby is transverse, he is lying horizontally in your uterus. Your doctor may try to manually turn him into a head-down position, but a cesarean section is usually needed.
If your baby is transverse, he is lying horizontally in your uterus. Your doctor may try to manually turn him into a head-down position, but a cesarean section is usually needed.http://www.pennmedicine.org/health_info/
Fetal Development: 32 weeks

Nowadays I can hear almost all sounds and noises outside my mom's belly..
I can feel the rays of sunlight when mum goes to her balcony and stands there ..she does not no how much I love that time..its so dark in here :(
I want to come out fast..i really do not like to stay all these ten months waiting and contemplating about different things..
Even when my pappa calls me from outside and touches me I feel so exited and want to come out at the very moment itself and play with him..he also gets same excited when he sees my head bulging out from my mom's belly..he acts like a child! and continues to speak to me in gibberish..so silly..hee hee!
I have gained alot of weight in the past few days..and gradually mom is becoming a little relaxed by this. Actuallu due to the fact of diabetes and diet etc she was not gaining weight to that extent in the past few weeks. My grand mom was worried herself and tried to convey her anxiety to mom..now she is also happy..
Grand mom ..wait ..still a lot of weight gain is still pending on my side..
Your Baby - 32 Weeks Pregnant
Pregnancy Week 32 Your baby sleeps approximately 90 to 95 percent of the day now. His skin has become thicker and he continues to become more of a pinkish color. Your baby's movements will peak this week. From now on they will change in quantity and quality. Most of the wrinkles are disappearing from your baby's face, and there may be a lot of hair on his head. The weight gain has been fairly incredible
recently. Your baby is now almost 4 pounds and is 17 inches long.
Your Body
Pregnancy Week 32 The discomforts of pregnancy may be wearing you down. Remember to rest as much as you can. There are many things you can do to help relieve some of these discomforts such as massage, relaxation techniques, stretching, exercise, proper posture and a healthy, balanced diet. Be sure not to take any sort of pain medication - even over the counter remedies such as Tylenol or Advil - without first discussing it with your doctor.
You may be wondering about what the birthing process will truly be like. Depending upon whom you ask, you may find yourself with varying examples. According to reports and research, approximately ten percent of women will report that labor is truly painful, while another ten percent will report no pain at all. Everyone else is somewhere in the middle of this spectrum. Your experience will differ from others as you may have a different pain threshold, and may choose to use or not to use any type of medications during birth. There are many factors that can affect the amount of pain you will experience during birth.
Your body is producing a hormone called relaxin. This hormone is responsible for loosening or relaxing the pelvis, making it more mobile during delivery. You may feel the effects of this hormone in your legs as you experience waddling. Don't worry; this is only temporary. And when it comes time to give birth, you will be very grateful it's there.
Your fundus is approximately four inches above your navel.
Common Pregnancy Symptoms in Week 32
- Breast Changes: tenderness, fullness, darkening of the areola
- Frequent Urination
- Constipation
- Heartburn or Indigestion
- Headaches
- Marks
- Itching
- Round Ligament Pain
- Hemorrhoids
Monday, June 14, 2010
Fetal Development: 31 weeks

Yay! I am 31 weeks ..Hoorray..
Do you understand what that means?
Now the countdown of weeks left can be done in one digit..Both me and mom are happy..
Your Baby's Development This Week
Your baby is probably around 15-16 inches in length and weighs in around 3-4 pounds.
That fat layer is still building up, and with it the skin tone will continue to become more pink and less transparent in appearance.
The brain is becoming more ridged and grooved and the nerves are growing at a tremendous rate. Already the baby is processing information gleaned from all five senses.
Feel like the baby is doing a little dance in response to music? Might not be so much a funny image as a reality. Research has shown that babies do move in rhythm and response to musical input.
Pregnancy Symptoms You May Feel During Week 31
Have you noticed a sticky yellowish substance leaking from your breasts? The presence or absence of it is perfectly normal. Some women will leak this first stage of milk in the weeks before birth, others will only notice it after baby's arrival.
Other leaking issues? You might find it embarrassing, but many expectant moms experience urine leakage when sneezing, or maybe laughing. Wearing a pantyliner may help. Kegel exercises will be helpful as well.
Another uncomfortable reality? Your internal organs are not quite where they used to be. Your bladder feels squished, your lungs stuffed up higher into your chest and the uterus is a whole four inches above the belly button now.
You may experience a feeling of not being able to get your breath, but rest assured baby is breathing just fine. To help you breathe easier, try to sit and stand up straight, and sleep on your side, propped on pillows.
Visit With the Obstetrician
Sometime after 28 weeks your physician may order a Fetal Nonstress Test. This is a simple noninvasive procedure done in around thirty minutes time. Two belts will be placed on mother's abdomen, one to measure fetal heart rate, the other to monitor contractions. The baby's heart rate should increase with fetal activity, and should decrease at rest. Occasionally baby decides to nap during the test, and should that happen, sometimes a little buzzer will be used to wake up baby. This test may be ordered should there be any question on the level of fetal activity, or if there is a possibility of placental function issues, or if this is a high risk pregnancy.
Preparing for Baby
You and your partner may want to check into infant CPR and first aid classes now, as part of your preparation for the new arrival. It's a good idea for anyone who will be around baby, including grandparents or babysitters. The classes are often short and will bring a peace of mind to worrying new parents. Knowing that you are prepared for emergencies will make you feel much more confident as a new parent.
Pregnancy Lifestyle
Are you getting your body ready for labor? There are exercises that are helpful in preparing for childbirth. First of all, doing Kegel exercises daily will definitely help with labor and after wards. Contract those muscles you use to shut off the flow of urine. Work on holding for five seconds at a time, working up to 10 seconds contracted with 10 seconds rest in between. You should do three sets of 10 a day. Other exercises are yoga type stretches, that are geared to pregnant women and aid in strengthening and stretching and relaxing your muscles, especially those you'll rely on most during birth.
http://www.thebabycorner.com/pregnancy-calendar/
Fetal Development: 30 weeks
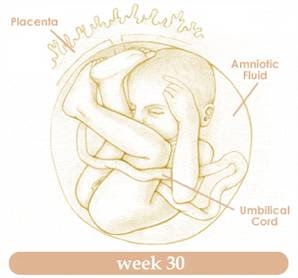
Though I am at present 31 weeks but still I have not told you what has happened when I was 30 weeks.
Hence have a look at the development status when fetus is 30 weeks and the mom is happy that she has reached the last leg of the journey :)
Your Baby:
Your baby now weighs almost 3 pounds - that like a head of a cabbage! And the length is about 17.7 inches.
The major development during this week is your baby's brain. Back then, the brain was just a smooth surface. Now it is characterized by grooves and indentations. This wrinkled appearance allows for the growth of the brain tissues. The bone marrow now begins to produce red blood cells.
The toenails are now beginning to grow.
Your baby's lanugo - which are the fine, downy hairs found in the body are starting to disappear. This is also the reason why premature babies have more lanugo than the full term ones.
Lanugo serves as a furry coat to protect your baby from extreme temperature. Since there are already baby fats and the brain can now function to regulate the body’s temperature, then there is no need for these hairs anymore. But a few can still be seen during childbirth.
Aside from the decreasing number of lanugo, the amniotic fluid also decreases in volume as the baby gets bigger- so she will need more space in the uterus to take up.
Your baby's eyesight continues to develop although it's not that clear yet. Even after birth, the baby can't see clearly until after two to three months. The vision then continnues to imporve throughout childhood. 29 weeks pregnant
, the baby's vision vision is still 20/400 out of the normal vision, which is 20/20.
Your body:
You may easily get tired and exhausted now that your baby weighs much heavier compared to the past months and especially if you have problems falling asleep.
Hormonal changes will make your ligaments more lax and the joints become looser. This is also in preparation for childbirth.
Another effect of the hormonal shifting is your mood swings. These may also be due to the uncomfortable symptoms that you are experiencing during the span of the pregnancy. These are just a normal part of pregnancy. But if you feel that the condition worsens from time to time and you can no longer handle it, then better consult your obstetrician or your psychologist, for you might be developing maternal depression.
You will still continue to have impaired circulation due to the fact that your growing uterus is continuing to put pressure on your veins and arteries.
The best position to allow better blood flow would be a left lying position when sleeping, which can aid in proper circulation to your organs and extremities.
The head of your baby is now putting pressure on your bladder, causing you to urinate more frequently. Your breast may become tender (again!) as they gear up for the production of milk.
You may notice that your heartburn is getting worse each week.
There are actually ways in which you can prevent heartburn like avoiding foods that are gastric irritants like spicy foods, fatty or fried foods, coffee, carbonated beverages, and also chocolates. Eat small yet frequent meals, and don't lie down while you are eating or right after a meal. Stress has also been associated with heartburn. So take time to relax and have frequent rest periods. You may also want to go to your health care provider if these things won't work.
http://www.easybabylife.com/
Betnosol Injection for lungs maturation:
I am getting ready to inhale and exhale on my own in my mum's womb. But still why would any one prescribe my mum to take Betnosol injection for my lungs maturation?
I really do not understand what these doctors are upto these days!
My mom's gynecologist does not want to take any chances with my lungs maturation. I think she is also worried for the fact if I am born premature before 34 weeks..then what!
Hence to make my lungs in a workable condition she is prescribing mom to take the dose of 3ampules each for 2 consecutive days, 24 hours apart.
I am trying mom to let her know that mom I am lots of hiccups and practicing my best to make my small lungs ready for the world outside so that when I come out I can smell the fragrance of my mom's body and also gets the smell of the mouth watering kebabs and fish which my dad loves to eat and brings home sometimes.
But forget about the what if scenarios and we will have to prepare our shelves for the shots.
Mom get ready and read these info before we proceed..
Betnesol Injections during pregnancy:
Betnesol, or betamethasone, is administered during pregnancy when preterm birth is a possibility. The steroid injection helps to produce surfactant in the baby's lungs, allowing them to inflate without sticking together. Normally, babies do not make this surfactant on their own until much later in pregnancy, around 32-35 weeks. Getting steroid injections into the mother at least 24 hours prior to a premature birth improves the baby's ability to breathe, reducing ventilation time and possibly reducing NICU time.
If your doctors are recommending this injection for you, they should have detected something that tells them your baby is at risk for premature birth. While fibroids can put you at risk for miscarriage and preterm labor, a fetal fibronection test (FFN) can more conclusively tell if this pregnancy in particular is at risk. If you have not had a positive FFN test, and you are not currently having preterm labor or carrying multiples, then you should ask for documentation of why this shot is being recommended for you and what your alternatives are. Betamethasone is not without risks; it can be lifesaving for premature babies, but it can have consequences on learning and development down the road.
---------------
How does it work?
Betnesol injection contains the active ingredient betamethasone sodium phosphate, which is a type of medicine known as a corticosteroid. Corticosteroid medicines are derivatives of the corticosteroid hormones cortisol and aldosterone that are produced naturally by the adrenal glands. They are often simply called steroids, but it should be noted that they are very different from another group of steroids, called anabolic steroids, which have gained notoriety because of their abuse by some athletes and body builders.
Corticosteroids have many important functions on every organ system. They affect the strength of heart muscle and its response to natural chemicals affecting heart rate. They affect the water and salt balance in the body and also enable the body to cope with stress. Stress includes changes in temperature, pain, fear, anxiety and illness. Stress can be hazardous if the body is not equipped to cope due to low levels of corticosteroids.
Corticosteroids allow us to respond to stress by increasing the rate and force of the heartbeat, increasing blood supply to essential tissues (muscle, heart, brain), increasing the body's supply of energy by raising blood sugar and by several other effects on body systems.
If the body's natural level of steroid hormones is too low because the adrenal glands are not producing enough hormones (a condition called adrenal insufficiency, for example in Addison's disease or following surgical removal of the adrenal glands), this can cause various symptoms, such as dizziness, fatigue, weakness, gut symptoms, depression and joint and muscle pain. It can also lead to collapse and death if the body is put under stress. Low blood levels of corticosteroids must be treated with replacement therapy to allow the body to function normally. This is usually acheived with a combination of hydrocortisone and fludrocortisone tablets.
Betamethasone is given by injection in situations where the levels of corticosteroids in the body suddenly become too low, causing shock and collapse. This might be due to many reasons, including abnormal stress in people with Addison's disease. This is an emergency situation and Betnesol injection is used to provide rapid control of symptoms.
Corticosteroid hormones are also involved in controlling inflammatory responses in the body. Betamethasone has an anti-inflammatory effect and is used to decrease inflammation in various different diseases and conditions.
Betamethasone decreases inflammation by acting within cells to prevent the release of certain chemicals that are important in the immune system. These chemicals are normally involved in producing immune and allergic responses. By decreasing the release of these chemicals in a particular area, inflammation and allergic reactions are reduced. Betnesol injection is used in serious or emergency situations when rapid control of symptoms is needed, for example in severe asthma attacks or severe allergic reactions such as anaphylaxis.
Betamethasone can also be injected directly into inflamed soft tissue, for example in tennis elbow, to decrease inflammation in that particular area.
What is it used for?
* Severe allergic reactions, such as anaphylaxis, angioedema or severe asthma attack.
* Severe drop in blood pressure causing dizziness, paleness and sweating (shock) due to surgical or accidental trauma or severe infection.
* Inadequate production of natural steroid hormones by the adrenal glands (acute adrenal insufficiency) due to abnormal stress in people with Addison's disease, Simmond's disease, people who have had their adrenal glands surgically removed, and people with underactive adrenal glands due to prolonged corticosteroid therapy.
* Local injection into inflamed soft tissue, such as tennis elbow, tenosynovitis, or bursitis.
* Injection into the eye to reduce inflammation in the eye.
Warning!
* This medicine must not be stopped suddenly if you have been given more than 1mg daily for more than three weeks; if you have been given high doses (more than 6mg) even if only for three weeks or less; if you have been treated with corticosteroid tablets or injections in the last year; if you had problems with your adrenal glands before treatment was started; or if you have been given repeated doses in the evening. In these situations this medicine can suppress the natural production of corticosteroids by the adrenal glands, which means that the body becomes temporarily reliant on the medicine. When it is time to stop treatment the dose should be tapered down gradually, to allow the adrenal glands to start producing adequate amounts of natural steroids again. However, in general Betnesol injection is not intended for long-term use and is unlikely to be used for longer than two or three days. If corticosteroid treatment is still needed after this you are likely to be switched to a corticosteroid taken by mouth where possible. Other steroids should also not be stopped abruptly.
* If you are having long-term or repeated treatment with steroids you will be given a steroid card that you should carry with you at all times. Show it to anyone who treats you (eg doctor, nurse, pharmacist, dentist, anaesthetist). The card contains details of your prescriber, type of steroid, dose taken and the duration of treatment. It's purpose is to act as a reminder that your medicine should not be stopped suddenly, and to provide information of your treatment to other people treating you. This is important because the effects that corticosteroids have on the body may affect other medical treatment you may be given. If you have an accident the card contains information that could save your life. You should also show your steroid card to anyone who treats you for three months after you stop treatment with steroids.
* Corticosteroids decrease the body's natural immune and inflammatory responses. They may increase your susceptibility to infections and can also mask the symptoms of infections, making you think they are less serious than they are. For this reason, it is important to consult your doctor if you get any signs of infection during treatment.
* If you have never had chickenpox you could be at risk of severe chickenpox while having long-term treatment with this medicine and should avoid close personal contact with people who have chickenpox or shingles (herpes zoster). You should also avoid contact with people who have measles. If you are exposed to people with these diseases either during treatment, or in the three months after stopping treatment, you should consult your doctor urgently, as you will need an injection of immunoglobulin to help you stop getting the diseases. This is very important as these diseases can be life-threatening in people treated with long-term corticosteroids.
* Corticosteroid treatment, especially with high doses, can alter mood and behaviour early in treatment. People may experience confusion, irritability, nightmares, difficulty sleeping, mood changes and depression, and suffer from delusions and suicidal thoughts. In a few cases these effects have also occured when corticosteroid treatment is being withdrawn. For this reason, it is important to let your doctor know if you notice any change in your mood or behaviour during treatment or when stopping treatment, particularly if you begin to feel depressed, or have any disturbing thoughts or feelings. Most of these problems go away if the dose is lowered or the medicine is stopped. However if problems do happen they might need treatment.
* Children and adolescents having long-term treatment with this medicine should have their growth regularly monitored.
Use with caution in
* Children and adolescents.
* Elderly people.
* Decreased kidney function.
* Liver failure.
* Peptic ulcer.
* Inflammation of the bowel and back passage (ulcerative colitis).
* Painful inflammation of small sacs or pouches in the wall of the gut (diverticulitis).
* People who have recently had a surgical procedure called intestinal anastomosis, which involves the joining together of ends of the intestine after a section has been removed.
* People with a history of blood clots in the blood vessels (thromboembolism).
* Heart failure.
* People who have recently had a heart attack.
* High blood pressure (hypertension).
* Diabetes, or a family history of diabetes.
* Underactive thyroid gland (hypothyroidism).
* Epilepsy.
* Glaucoma, or a family history of glaucoma.
* Current severe psychiatric illness, or a personal or family history of psychiatric illness, including depression, manic depression or schizophrenia.
* History of psychiatric illness caused by the use of a corticosteroid.
* Osteoporosis.
* Women who have passed the menopause.
* Abnormal muscle weakness (myasthenia gravis).
* People who have previously experienced muscle disorders (myopathy) caused by steroids.
* People with a history of tuberculosis (TB).
* Herpes simplex virus infection of the eye.
* People with a low level of potassium in their blood (hypokalaemia).
Not to be used in
* People with widespread infection, unless this is being treated with specific anti-infectives.
* Corticosteroids should not be used for the management of head injury or stroke because they are unlikely to be of benefit and may even be harmful.
* Betnesol injection should not be injected directly into tendons.
This medicine should not be used if you are allergic to one or any of its ingredients. Please inform your doctor or pharmacist if you have previously experienced such an allergy.
If you feel you have experienced an allergic reaction, stop using this medicine and inform your doctor or pharmacist immediately.
Pregnancy and breastfeeding
Certain medicines should not be used during pregnancy or breastfeeding. However, other medicines may be safely used in pregnancy or breastfeeding providing the benefits to the mother outweigh the risks to the unborn baby. Always inform your doctor if you are pregnant or planning a pregnancy, before using any medicine.
* When administered for long periods or repeatedly during pregnancy, corticosteroids may increase the risk of slowed growth in the developing baby. They may also cause the baby to make less of its own steroid hormones after birth, but this usually resolves on its own and rarely causes any problems. When used during pregnancy betamethasone may also temporarily reduce the baby’s heart rate and body movements. As a result this medicine should be used with caution during pregnancy, and only if the expected benefit to the mother is greater than any possible risk to the developing baby. Seek further medical advice from your doctor.
* This medicine passes into breast milk. It should be used with caution in mothers who are breastfeeding and only if the benefits to the mother outweigh any risks to the nursing infant. Lower doses taken by the mother are unlikely to significantly affect the baby, but if the mother is taking high doses for long periods of time, the medicine could cause the baby's adrenal glands to make less of their own steroid hormones. Seek medical advice from your doctor.
Side effects
Medicines and their possible side effects can affect individual people in different ways. The following are some of the side effects that are known to be associated with this medicine. Just because a side effect is stated here does not mean that all people using this medicine will experience that or any side effect.
* Raised blood sugar level.
* Increased appetite and weight gain.
* Increased susceptibility to infections and increased severity of infections (see warnings above).
* Effects on the gut, such as indigestion or abdominal bloating, nausea, ulceration in the stomach or intestine, inflammation of the pancreas (pancreatitis).
* Ulceration or thrush infection in the throat.
* Muscle weakness or wasting.
* Thinning of the bones (osteoporosis) and increased risk of breaking a bone.
* Effects on the skin, such as skin thinning, impaired healing, acne, bruising, stretch marks, increased sweating, change in pigmentation, increased hair growth (hirsutism).
* Psychiatric reactions, such as mood changes (including irritability, depression and suicidal thoughts), psychotic reactions (including mania, delusions and hallucinations), anxiety, confusion, memory loss, sleep disturbances (see warning above).
* Cushing's syndrome, characterised by a moon face.
* Menstrual disturbances.
* Decrease in the production of natural steroids by the adrenal glands (adrenal suppression - see warning above).
* Effects on the eyes, such as raised pressure inside the eye (glaucoma), cataracts.
* Slowed growth in children and adolescents.
* Hiccups.
* Blood clots in the blood vessels (thromboembolism).
The side effects listed above may not include all of the side effects reported by the medicine's manufacturer.
For more information about any other possible risks associated with this medicine, please read the information provided with the medicine or consult your doctor or pharmacist.
How can this medicine affect other medicines?
It is important to tell your doctor or pharmacist what medicines you are already taking, including those bought without a prescription and herbal medicines, before you start treatment with this medicine. Similarly, check with your doctor or pharmacist before taking any new medicines while being treated with this one, to ensure that the combination is safe.
Betamethasone may increase blood sugar levels and so may oppose the blood sugar lowering effects of antidiabetic medicines. People with diabetes may need an increase in their dose of insulin or antidiabetic tablets.
Betamethasone may enhance the anti-blood-clotting effect of anticoagulant medicines such as warfarin. People taking anticoagulant medicines in combination with betamethasone should have their blood clotting time (INR) regularly monitored, particularly after starting or stopping treatment with betamethasone and after any dose changes.
If betamethasone is used in combination with non-steroidal anti-inflammatory drugs (NSAIDs) eg ibuprofen, there may be an increased risk of side effects on the gut, such as stomach ulceration and bleeding.
Betamethasone may decrease the blood levels of salicylates such as aspirin. When betamethasone is stopped, this may result in excessive levels of the salicylate, unless the dose is readjusted.
The following medicines may increase the removal of betamethasone from the body, thus reducing its effects. You may need a larger dose of betamethasone if you are also taking any of these medicines:
* barbituates, eg amobarbital, phenobarbital
* carbamazepine
* phenytoin
* primidone
* rifabutin
* rifampicin.
The effect of corticosteroids may be reduced in the three to four days following use of mifepristone.
The following medicines may reduce the removal of betamethasone from the body and so may increase its effects or side effects:
* ciclosporin (betamethasone may also increase the blood level and risk of side effects of ciclosporin)
* itraconazole
* ketoconazole
* macrolide-type antibiotics, eg erythromycin
* protease inhibitors, eg ritonavir.
Betamethasone may decrease the body's immune response. This means that vaccines may be less effective if given during treatment, because the body does not produce sufficient antibodies. Live vaccines may cause serious infections. Live vaccines include: measles, mumps, rubella, MMR, BCG, chickenpox, oral polio, oral typhoid and yellow fever. These should not be given to people whose immune system is underactive due to treatment with this medicine.
Corticosteroids can cause fluid and salt retention and so may oppose the effects of antihypertensive medicines used to treat high blood pressure, and diuretics such as furosemide. However, betamethasone is much less likely than other corticosteroids to have this effect.
Corticosteroids can also lower the amount of potassium in the blood, though this is much less likely with betamethasone than with other corticosteroids. However, there may be an increased chance of the level of potassium in the blood falling too low (hypokalaemia) if betamethasone is used in combination with the following medicines:
* acetazolamide
* amphotericin
* beta agonists, eg salbutamol, salmeterol, terbutaline
* carbenoxolone
* potassium-losing diuretics, eg furosemide, bendroflumethiazide
* theophylline.
Other medicines containing the same active ingredient
Betamethasone has many different uses and comes in many different forms. The factsheets below contain information about betamethasone used in various areas of the body.
-----------------------
Steroid Injection for Fetal Lung Development
Injections of corticosteroids for fetal lung development has been praised as one of the best advances in fetal medicine in the 90s. Since 1994 the National Institutes for Health and other professional organizations have encouraged their use in promoting the development of fetal lung development in moms who were at risk for preterm labor or birth.
Betamethasone and dexamethasone are the two most commonly used steroids. The average protocol was to give to intramuscular injections (IM) 24 hours apart. Some practitioners also choose to continually repeat the dosages every week until the birth. The injections had to be given 24-48 hours prior to the birth for maximum effect. They were also best used between weeks 24 and 34 gestation.
The use of the steroids provided benefits for the lung development in the premature infants to reduce the risk of respiratory distress syndrome (RDS) as well as to reduce the risk of intracranial hemorrhaging and some other potential benefits.
However, recent studies say that the benefits of multiple doses is questionable, particularly in light of potential risks. Citing the "limited quality" of the studies of multiple doses and the potential disadvantages the National Institute of Health issued a statement of August 18th that a single dose was sufficient in achieving the benefits desired.
Potential down sides to multiple doses can include: psychomotor delays, behavioral problems and the fact that the effects on neonatal mortality aren't known between the single and multiple dose courses. In separate findings by an Israeli study it was also noted that there is an increase in maternal infection with the use of steroids, so limiting doses may help with this side effect as well.
The steroid injection is to help mature the baby's lungs in case of premature delivery. Yes it has potential side effects (EVERY medication has potential side effects...there's no free ride when it comes to pharmacology). It develops the fetal lungs early because it sets up a very stressful environment for the baby. Decreased birth weight, decreased brain size, abnormal brain development, adverse effects on the fetal immune system, are just some of the potential side effects. Steroid injections for fetal lung development should not be taken lightly. It should be used only for cases where premature delivery is expected and the potential benefits outweigh the potential side effects.
I don't know why the doc told her that one injection is harmful but more than one is not. Sounds like she didn't really understand what was being explained to her.
http://www.naturallycurly.com/curltalk/showthread.php?t=27953
Antenatal corticosteroids for fetal lung development
Examples
betamethasone Celestone Soluspan dexamethasone Dalalone Decadron
How It Works
Betamethasone and dexamethasone cause an immature fetus's lungs to produce a compound called surfactant. A full-term baby's lungs naturally produce surfactant, which lubricates the lining of the air sacs within the lungs. This allows the inner surfaces of the air sacs to slide against one another without sticking during breathing. Premature infants whose lungs have begun producing surfactant have an improved ability to breathe on their own, or with less respiratory treatment, after birth.
When preterm birth between 24 and 34 weeks of pregnancy (gestation) is expected within 7 days, betamethasone or dexamethasone is given to the mother in order to affect the fetus. Betamethasone is given in 2 injections, 24 hours apart. Dexamethasone is given every 12 hours for 4 doses.
If delivery does not occur within 7 days of treatment, the injections should not be repeated. Recent guidelines issued by the National Institutes of Health discourage such repeat courses of treatment, based on concerns about fetal harm from repeat treatments.1
Why It Is Used
Corticosteroids are considered standard treatment for women who are 24 to 34 weeks pregnant and may deliver within the next 1 to 7 days, with or without preterm premature rupture of membranes (pPROM).1
Betamethasone and dexamethasone are corticosteroids, also called glucocorticoids, that are given before birth (antenatally) to speed up a preterm fetus's lung development. Either is used when a mother is in preterm labor and birth may occur in 24 to 48 hours. This helps prevent the occurrence of respiratory distress syndrome (RDS) and related complications following premature birth.
Many infants born at 33 to 34 weeks' gestation have sufficient lung maturity to breathe on their own. However, considering the low-risk, high-benefit nature of this treatment, corticosteroids are typically used up to 34 weeks of pregnancy.
WebMD
Betamethasone is often used in patients with premature labor at about 26-34 weeks' gestation to stimulate fetal lung maturation The benefits of this therapy are: Reduction in incidence of respiratory distress syndrome (RDS) Decreased severity of RDS if it occurs Decreased incidence of, and mortality from, intracranial hemorrhage Increased survival of premature infants Betamethasone crosses the placenta to the fetus . The drug is partially metabolized (47%) by the perfused placenta to its inactive 11-ketosteroid derivative, but less so than other corticosteroids, although the differences are not statistically significant .
In patients with premature rupture of the membranes (PROM), administration of betamethasone to the mother does not always reduce the frequency of RDS or perinatal mortality . An increased risk of maternal infection has also been observed in patients with PROM treated with corticosteroids . In a study comparing betamethasone therapy with nonsteroid management of women with PROM, neonatal sepsis was observed in 23% (5 of 22) of steroid-exposed newborns vs. only 2% (1 of 46) of the non-steroid-exposed group . A 1985 study also found increased neonatal sepsis in exposed newborns who were delivered more than 48 hours after PROM, 18.6% (14 of 75) vs. 7.4% (4 of 54) of nonexposed controls . In addition, moderate to severe respiratory morbidity was increased over that in controls, 21.3% vs. 11.1%, as well as overall mortality, 8% vs. 1.8% . Other reports, however, have noted beneficial effects of betamethasone administration to patients with PROM with no increase in infectious morbidity (15,23,24,). In women colonized with group B streptococci, the combined use of betamethasone and ampicillin improved the outcome of preterm pregnancies with PROM .
Betamethasone therapy is less effective in decreasing the incidence of RDS in male infants than in female infants . The reasons for this difference have not been discovered. Slower lung maturation in male fetuses has been cited as a major contributing factor to the sex differential noted in neonatal mortality. Therapy is also less effective in multiple pregnancies , even when doses have been doubled . In twins, only the first-born seems to benefit from antenatal steroid therapy .
An increased incidence of hypoglycemia in newborns exposed in utero to betamethasone has been reported . Other investigators have not observed this effect.
In the initial study examining the effect of betamethasone on RDS, investigators reported an increased risk of fetal death in patients with severe preeclampsia. They proposed that the corticosteroid had an adverse effect on placentas already damaged by vascular disease. A second study did not confirm these findings .
A case of suspected betamethasone-induced leukemoid reaction was observed in an 880-g, 30-weeks'-gestation female infant whose mother received 12 mg of betamethasone 4 hours prior to delivery . A second case, in a female infant born at 25-26 weeks' 71 hours after betamethasone, was published in 1997 . Within about 710 days, the white blood cell count had returned to normal in both infants. A 1984 study examined the effect of betamethasone on leukocyte counts in mothers with PROM or premature labor . No effect, as compared to untreated controls, was found in either group.
A case of acute, life-threatening exacerbation of muscular weakness requiring intubation and mechanical ventilation was reported in a 24-year-old woman who was treated with betamethasone, 12 mg IM, to enhance fetal lung maturity at 32 weeks' gestation . The onset of symptoms occurred 30 minutes after the corticosteroid dose. The authors attributed the crisis to betamethasone (adrenocorticosteroids are known to aggravate myasthenia) after other potential causes were ruled out. The infant was delivered by emergency cesarean section and, except for the typical problems related to prematurity, he had a normal hospital course.
Hypertensive crisis associated with the use of ritodrine and betamethasone has been reported . Systolic blood pressure was above 300 mm Hg with a diastolic pressure of 120 mm Hg. Although the hypertension was probably caused by ritodrine, it is not known whether the corticosteroid was a contributing factor.
Breast Feeding Summary
No reports describing the use of betamethasone during human lactation have been located. The molecular weight (about 435 for the acetate salt and about 517 for the sodium phosphate salt) are low enough, however, that excretion into milk should be expected.
http://drugsafetysite.com/betamethasone/
What should I watch for while taking betamethasone?
Visit your prescriber or health care professional for regular checks on your progress. If you are using corticosteroids for a long time, carry an identification card with your name, the type and dose of corticosteroid, and your prescriber's name and address. Do not suddenly stop using betamethasone. You may need to gradually reduce the dose, so that your body can adjust. Follow the advice of your prescriber or health care professional.
If you receive corticosteroids for a long time, avoid contact with people who have an infection. You may be at an increased risk from infection while receiving betamethasone. Tell your prescriber or health care professional if you are exposed to anyone with measles or chickenpox, or if you develop sores or blisters that do no heal properly.
People who are taking certain dosages of betamethasone may need to avoid immunization with certain vaccines or may need to have changes in their vaccination schedules to ensure adequate protection from certain diseases. Make sure to tell your prescriber or health care professional that you are taking betamethasone before receiving any vaccine.
If you are diabetic, betamethasone can affect your blood sugar levels. Check with your prescriber or health care professional if you need help adjusting the dose of your diabetic medicine.
If you are receiving betamethasone injections every day, you may need to watch your diet. Your body can also lose potassium while you receive this medicine. Ask your prescriber or health care professional about your diet, especially about your salt intake.
If you are going to have surgery tell your prescriber or health care professional that you are receiving betamethasone, or have taken it within the last 12 months.
If betamethasone has been injected into one of your joints, do not put too much stress on the joint for a while. Talk to your prescriber or health care professional about how much you can use the joint while it is healing.
Elderly patients have an increased risk of side effects from betamethasone.
Betamethasone can interfere with certain lab tests and can cause false skin test results.
What side effects may I notice from receiving betamethasone?
Side effects that you should report to your prescriber or health care professional as soon as possible:
• bloody or black, tarry stools
• confusion, excitement, restlessness, a false sense of well-being
• eye pain, decreased or blurred vision, or bulging eyes
• fever, sore throat, sneezing, cough, or other signs of infection
• frequent passing of urine
• hallucinations (seeing and hearing things that are not really there)
• increased thirst
• irregular heartbeat
• menstrual problems
• mental depression, mood swings, mistaken feelings of self-importance, mistaken feelings of being mistreated
• muscle cramps or muscle weakness
• nausea, vomiting
• pain in hips, back, ribs, arms, shoulders, or legs
• pain, redness, inflammation or scarring at the injection site
• rounding out of face
• skin problems, acne
• stomach pain
• swelling of feet or lower legs
• thin or shiny skin at the injection site
• unusual bruising or red pinpoint spots on the skin
• unusual tiredness or weakness
• weight gain or weight loss
• wounds that will not heal
Side effects that usually do not require medical attention (report to your prescriber or health care professional if they continue or are bothersome):
• headache
• increased appetite
• increased sweating
• nervousness, restlessness, or difficulty sleeping
• unusual increased growth of hair on the face or body
http://www.answers.com/topic/betamethasone-injection
Betamethasone is a corticosteroids, and as such can cause the following side effects:
Increased thirst and urination, lethargy, increased appetite, abortion during pregnancy, immune suppression (and thus more susceptible to other illnesses), muscle weakness and possible atrophy, stomach ulcers, diarrhea, panting, and possible bone weakness.
Now, keep in mind, these side effects are often rare, except for the increased drinking, urinating and eating. Also, these are much more likely to be seen in long term use, not one injection.
Read more: http://www.justanswer.com/questions/